
(last updated Sept 2014)
Coming Back from a Broken Hip
My long road to recovery from hip fracture surgery and soft tissue injuries after a bicycling accident
Saturday, July 23, 2005
On July 23, 2005 my right hip was fractured during an 80-mile bicycle ride on the roads of the Adirondack mountains. The cyclist in front of me hit something in the road, lost control of his bike and slid into me from the left side, taking both my wheels out and causing my right side to slam into the pavement. I was taken for a long ambulance ride to the nearest hospital where I was admitted after x-rays indicated a non-displaced intertrochanteric fracture of the right hip. The fracture was surgically repaired the following day by installing a compression hip screw and plate (see pictures below), anchored by 3 screws into my femur.
I've found very little information on what to expect in the long recovery from this injury, either from my doctors or from the internet. My naive expectations of a straightforward recovery over the course of a few months were not realized, so I thought I'd post a detailed account of my experience for the benefit of others who unfortunately experience a similar mishap. Ken Kifer posted the only other account I could find that was truly very helpful. At the bottom of this page, after the chronology, is a summary of what I learned through this ordeal. It's probably worth mentioning that I'm middle-aged (although "young" for my age), athletic, and fairly svelte (5'10" 140lbs).
Hospitalization:
After the accident, I spent 6 days in the acute care hospital and another 6 days in a rehab hospital. Before they performed the surgery, suffice it to say that any movement of the bad leg was absolutely excruciating. They had me out of bed on crutches the day after surgery, and I managed fairly well. However, I had a few fainting spells in the acute hospital - they occurred soon after starting a walking episode and were accompanied by very low BP. This was almost certainly due to blood loss in the accident and surgery combined with lingering effects of the general anesthetic and pain medication, although the hospital insisted on putting me through every diagnostic test imaginable (2CAT scans, EEG, etc).
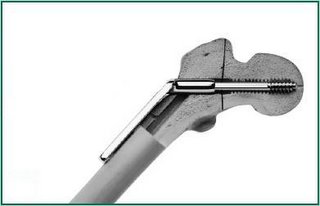 On the left is a photo of the compression hip screw and plate that was implanted in my right hip. The lower part of the plate that runs snug along the femur is secured by 3 screws (not shown) through the femur. (See further below for an additional photo of the hardware with screws.)
On the left is a photo of the compression hip screw and plate that was implanted in my right hip. The lower part of the plate that runs snug along the femur is secured by 3 screws (not shown) through the femur. (See further below for an additional photo of the hardware with screws.)
I was on a morphine pump for pain for the first 48 hours and then on oral percocet. I didn't use much of it because I wasn't really in that much pain after the surgery. One side note is that the general anesthetic combined with the opiate pain medication had a marked effect of depressing smooth muscle function - in other words, your eliminative functions really slow down. Morphine also have a strange nightmarish effect on your dreams. I did have a fair amount of muscle spasms in the hip, especially during walks on crutches. I was put on flexoril and this calmed down the spasms. After about a week or so, the spasms were gone.
I figured out how to grab my right leg with my good left leg, cradling it with the left foot. This is an important skill, because it took more than a month for me to be able to swing my right leg down from the bed using the muscles in the right leg. It was also really tough at first to put my right shoe on and to put pants on.
Physical therapy began in the hospital soon after the surgery. The therapy routine became much more serious when I got to the rehab hospital. There's a clear intention to get you independent so you can go home. It's a combination of strengthening, stretching, and practice simulating household environment (stairs, shower, etc).
What was especially disconcerting was the almost total inability to bend my knee. My quads and leg felt as stiff as a board. This was to be my nemesis for the coming months. From the little I could find out, the degree of stiffness in knee flexure that I experienced was quite unusual. It was later suggested that the knee stiffness was probably a result of the trauma suffered from the impact to the soft tissues of my leg and not the hip fracture itself.
Release:
On August 3, I was released from the Rehab hospital. Before release, they removed the staples from the surgical incision and applied steri-strips. This is normally done at 14 days post-op and in retrospect, it was a mistake to remove them a few days early because the wound wasn't 100% closed. They also trained me to give myself injections of anti-coagulant, which would be continued up until 4 weeks post-op. This was the only medication I was taking.
After returning home, it suddenly became apparent how much effort it took to get around the house and do all the little things when you're living alone. On August 4, I became aware of increasing edema/swelling in my leg. By the evening, even my ankle lost all definition and I was worried about the possibility of infection. I spent 5 hours in the ER waiting for a doctor to look at me and tell me to go home. In retrospect, I should have been wearing the compression stocking on the bad leg and staying off the leg a lot more at this early stage. After a night in bed, the swelling had subsided quite a bit.
On August 5, I went to stay with my sister for a week. I really wasn't ready to go it alone and the extra week of taking it easy was exactly what was needed. During this time, I religiously performed the exercises prescribed by the rehab hospital PT. The knee remained very stiff. After I returned home the next week, I discovered that I had no trouble driving. I started physical therapy sessions 2-3X per week.
Around the 3rd or 4th week I learned a trick to help with sleeping. Up until then I was sleeping exclusively on my back. The trick is to use a second pillow as a prop. When sleeping on the unaffected side, put the pillow between your knees. When sleeping on the affected side, put the pillow under your hip. And eventually I started to also use the 2nd pillow when sleeping on my back, placing it under my knee.
Physical Therapy:
The main focus was to regain knee flexibility. At first the prime exercise was the "wall slide." I would lay on my back on a table pushed against the wall. I placed my foot on the wall with my upper thigh perpendicular to the table and try to slide my foot down the wall and flex my knee more and more. The therapist would come over after about 10 minutes and assist the flexure (ouch). If I could attain about 120 deg of flexure, I could advance to the stationary bicycle. At first on the bike, I had to keep the seat quite high with my heel on the pedal to minimize knee flexure. The first few pedal strokes were fairly painful on the upstroke of the bad leg. I would do about 10 minutes of easy pedaling. After a couple of weeks, the therapist added another regimen of stretching between the wall slides and bicycle. I would lay prone on the table and he would flex my knee from the back and push my heel toward my butt. New horizons of pain were continually uncovered.
There were both noticeable steps forward and backward during my physical therapy. As I write now, I am in the 5th week of therapy. I have had two "bad" sessions, where I was in pain afterward, my knee flexion ability took a few days to recover, and I had to take a few days off from therapy. I had one "aha" in therapy Sept.8, where my muscles seemed to wake up and I could suddenly walk unaided with hardly a limp. This was followed by 3 days of walking without any crutch, including stairs. I even managed two easy bike rides 9/10 and 9/11. Unfortunately, one of the bad sessions immediately followed and I regressed to needing the crutch after my quads seemed to significantly weaken due to pain.
Week 6: I continue to be amazed at how quickly the stiffness in the knee and quads return after stretching them. The stiffness is really felt during the stretching as well. After my knee reaches about 90 deg, it is stiff, stiff, stiff. I can continue to push it past 90 degrees - it just becomes increasingly painful. So during the therapy sessions, it is a test of how much pain I can endure translating into how far we're gonna get the knee stretched today. The last session we just went too far and I knew it immediately after I got off the table - the leg hurt, and I was limping.
Around the 5th week post-op, the internal swelling must have subsided because I was suddenly much more aware of the hardware (plate) inside my leg. I started feeling a continual pressure and irritation, as if there was something in my pants pocket. The irritation seems aggravated by a lot of activity. When I walk, there is a constant feeling of slight irritation over the hip plate. The orthopedist says it will probably eventually subside, but if it doesn't, the hardware can be removed. 8 weeks post-op and the orthopedist says I'm doing fine and that it will take 6-12 months for the leg to feel almost normal.
Week 7: In the crash, the bike fared much better than I did. The front wheel was taco'd beyond repair, the bar tape was shredded and the STI levers were badly scratched. I had a new front wheel built, retaped the bars, replaced my helmet and gloves and gingerly ventured out on a 7 mile slow, flat bike ride. There was quite a bit of discomfort on every upstroke of the right leg for the first 10-15 minutes, but otherwise everything was fine. I went out again the next day and the following weekend as well. On my 4th ride of 14 miles, the discomfort was markedly reduced and I started to give just a little bit of effort beyond merely spinning slowly. Afterwards, I realized that my right leg was starting to feel like a leg again. The modest exercise seemed very beneficial. What discomfort there was during the ride, was more in the knees rather than the quads.
Week 8: Now at the 8 week mark, it seems that after a knee flexing session, the stiffness doesn't return so fast or so completely. And when I start a knee flexing session, I get to the 120-130 degree flex much more quickly, without taking 10-15 minutes to work up to it.
There was a pronounced bump in the contour of my hip, caused by the hardware underneath. I was resigned to this as a slight permanent deformity. After 8 weeks, I suddenly realized that the bump had almost completely disappeared, much to my relief.
Week 9: I realized something else about physical therapy. The agressive stretching session is followed by a few days of sore muscles/hipjoint. This soreness is also experienced as weakness (limping) - the body is naturally defensive about the soreness & stress on the muscles/tendons/joints and you feel weak. This week the therapist was able to bend my knee back to within 2 finger widths of my butt, so the flexibility is coming along. For some time afterwards, the area on my leg directly superior and superior/lateral to the knee cap was very sore. In addition to the hip flexors, extendors, abductors, and adductors, I've also added the internal rotators to the daily strengthening exercises.
Week 10 (early October): I went through another sore/painful few days after the last therapy session and after doing a 20-mile bike ride. I saw the surgeon again, who was very happy with the progress. He suggested stopping the physical therapy for a few weeks and see how it goes. He wasn't concerned with recapturing the last few percent of range-of-motion on the knee and was happy I could bike again without discomfort. When I told him that there was irritation over the plate whenever I walked for any distance, he said that we might have to consider removing the plate in another 3-6 months.
November 23, 2005
Since my week 10 posting, the inflammation in my hip centered around the hardware gradually increased to the point where I ceased all exercise activity completely and had to go back on crutches a few times to take the weight off the leg. I received anti-inflammatory injections into the hip to try and tame the inflammation around the hardware. This was a good faith effort by my surgeon to avoid surgical removal of the hardware. He intimated that he would consider removing the hardware in January or February if the injections didn't help. They didn't and my limp slowly got worse.
December 30, 2005 - Surgery #2
I had in-patient surgery to remove the hardware and stayed in the hospital for 24 hours. The surgeon put a drainage tube up into the femoral neck that came out of my leg into a bag. This was removed when I was discharged the next day. I arranged to receive the hardware that was removed. The surgeon told me that they had to chip away bone that had already started to grow around the hardware in order to remove it.
day. I arranged to receive the hardware that was removed. The surgeon told me that they had to chip away bone that had already started to grow around the hardware in order to remove it.
I was able to get around well enough the day after surgery so that I could fend for myself at home. I took it easy for a week at home and then returned to work. It's now 3 weeks later and I'm still feeling a fair amount of pain and soreness. I started to walk a bit without crutches about 2-1/2 weeks after surgery. But I've already aggravated the pain by some gentle cycling on a trainer and it was quite painful for several days after. There was a sizeable hematoma from the surgery and it's now smaller but the area is still swollen after 3 weeks and causing some discomfort. Sleep is a bit challenging because every night the hip starts bothering me after a few hours of sleep. I spend the rest of the night constantly changing positions between sleeping on my back and on my left side, and use a second pillow under my knees or between my knees.
It will take a few months for the holes in my femur to fill in that were left by the hardware, so strenuous cycling will have to wait till the spring at least.
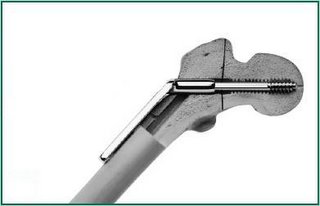
The photo shows the actual removed hardware in the proper orientation as it was in my leg. The material is either stainless steel or titanium and it weighed a hefty 6 oz. I'm VERY glad that it's out of my leg now.
January 27, 2006
It's now 4 weeks after the removal surgery and I've gone back on crutches in an effort to give the hip the best chance of recovery. It still feels quite aggravated from the 15 minutes of easy trainer cycling I did five days ago.
On the advice of my surgeon, I began physical therapy again on Feb 8. I'm getting iontophoresis (electrical current drives anti-inflammatory medication into the tissues) as well as hot/cold, stretching, ultrasound, massage, and some exercises. The hip still can't take much exercise without being aggravated for a few days afterward.
February 23, 2006
It now appears that the hip still needs more time (rest) before beginning any exercise. It's eight weeks after hardware removal surgery and seven months since the accident. It's hard to accept that an injury could need this much time, but evidently it does. I honestly haven't experienced any improvement as a result of the physical therapy begun two weeks ago. In fact, it seems to have only aggravated the leg. I stopped the physical therapy.
March 9, 2006
I tried 5 minutes of very easy spinning on my trainer and once again it greatly aggravated my hip. It's now 10 weeks since hardware removal. I went in and saw my local orthopedist, trying to find out why the hip is so intolerant of exercise. He told me what I'm experiencing is normal and it's just too soon after the hardware removal surgery. He said I probably will need another 3 months (gulp) before riding much and 6 months to really heal completely. He also warned that I may always have a little pain in the hip in the future. He also said that the fact that the incision scar is still red indicates there's still a lot of inflammation/rebuilding going on. When the scar turns white, that will be a sign that healing has progressed (?!).
April 3, 2006
My condition is still about the same - slight exercise results in ~5 days of mild-moderate aggravation. I visited my GP and we discussed the fact that these injuries normally take about 12 months to heal. But what if, I conjectured, after 12 months the hip still hurts and then we look and find another underlying injury? My GP concurred and suggested we go ahead and get an MRI taken to rule out additional injury. The resulting MRI report indicated that there's still a fracture, which caused some confusion. My surgeon sent the MRI to be re-read in hope of determining whether it's the original fracture that is still healing or whether there might be a new stress fracture. While I wait for the news, the surgeon has put me back on crutches to unweight the hip. He was also concerned because I had a pronounced limp due to aggravation from an easy 1 mile hike three days earlier.
Okay, ten days later I heard back from my surgeon. He went over the films with a respected radiologist and they decided there's nothing to worry about on the MRI. He wants me to rest the hip another 3-4 weeks before attempting some easy exercise.
April 16, 2006
My GP, who was actually the one who ordered the MRI, asked a radiologist expert in bones/joints to also re-read the MRI. This radiologist thinks there may be a problem in the hip joint itself. I am scheduled for another MRI with contrast injected into the hip (arthrogram) along with local anesthetic (marcaine) to help confirm the joint is the source of the pain. I guess the good news is that they may have found the underlying problem that has delayed my recovery for so long. I know it's premature, but I've starting researching minimally invasive arthroscopic hip surgery, which is only performed by a select few orthopedists nation-wide. My experience clearly supports the need to take a very active role in one's treatment. You should handpick your radiologist BEFORE you have an MRI performed. You just CANNOT defer the medical decisions and choices to your doctors. Sometimes you have to question their diagnosis or lack thereof.
April 27, 2006
I did some exercise to aggravate the hip leading up to the exam. When I met with the radiologist before the exam, he actually felt that the arthrogram MRI was unnecessary but he wanted to do the injection into the joint. Bottom line - I felt zero relief after the injection, which essentially all but rules out the hip joint as the source of my current difficulty in tolerating exercise. Back to square one. I made an appointment to see a new orthopaedist in 3 weeks and I'll give him a shot at cracking the mystery.
May 16, 2006
The new (#3) orthopedist said it was either trochanteric bursitis or iliotibial band tendonitis. He said the fracture/surgery may have resulted in permanent issues with the soft tissue to bone interface. First thing to try was a cortisone injection into the bursa, which he duly performed. He recommended stretching of the iliotibial band and trying some walking/swimming in 3-4 days.
May 31, 2006
The cortisone injection into the bursa didn't help at all. #3 orthopaedist seems less definite on what the problem may be and he essentially threw in the towel and told me to just give it time.
I've given up on the orthopedists in the surrounding area. I've contacted highly regarded orthopedists in Colorado and New York City.
I tried exercising easily for a few minutes on a NordicTrack, but the usual hip aggravation set in 1-2 days later.
June 23, 2006
After phone consultations with the Colorado orthopedist, I had another MRI performed at the Hospital for Special Surgery in NYC. They clearly saw significant scar tissue and adhesions between the hip musculature and tendons. I saw an orthopedist there (#4) and he wants to first try physical therapy and if unsuccessful, endoscopic surgery to alleviate the scarring and adhesions. This is probably the problem that started back in October, but failed to be diagnosed by my local orthopedists. He also prescribed an ultrasound-guided injection into the trochanteric bursa. This injection definitely resulted in some relief, and I'm apt to believe that the previous "blind" injection one month earlier missed the mark.
On June 26, I went into physical therapy again and the therapist is using ultrasound and agressive massage (release) therapy in an attempt to break up the scar tissue - also plenty of stretching and hot/cold etc. I'm also seeing a chiropractor who is doing Active Release Technique in an attempt to break up the scar tissue and adhesions. That's 4 therapy sessions per week.
August 1, 2006
The therapy continues. Based on recommendation by a few locals, I saw another orthopedist (#5) who says my case isn't that unusual despite that fact that in my research after my initial accident, I never read anywhere that it can take years to come back from a broken hip and that soft tissue issues were so difficult. He said DON'T go in for more surgery in an effort to resolve the adhesions. He said that I should expect some pain and discomfort and slowly resume physical activity and to try another anti-inflammatory medication.
The next day my active release therapist/chiropractor told me to do yoga and look toward stretching/strengthening my entire body rather than jump into an exercise routine that only worked my upper or lower body. He also encouraged cross-training.
For ten months, I had thought there must be one specific underlying problem that needed correcting and then I would be "okay." I now realize it's going to be a VERY slow road back and I'll have to learn to tolerate some level of pain for some time to come. This was confirmed by the orthopedist on August 1, but none of the doctors up until that time expressed this view. For the first 10 months, none of the doctors brought up the possiblity of soft tissue injury either.
September 7, 2006
I cut back on my therapy to one session of Active Release Technique per week, but have been doing 3 yoga classes per week. The hip finally feels like it is really starting to come back to life. It doesn't feel "normal" like the good hip, but it is feeling strong and capable. I do an occasional vigorous 2-mile hike, although it's ususally a bit sore for a couple of days after. I take 600-800mg ibuprofen when I do experience soreness. I tried a few 5-minute sessions on the bike trainer, but there still seemed to be a residual achiness for a few days afterward. However, on the insistence of my chiropractor, I did an easy 30-minute bike ride yesterday.
September 13, 2006
After a few days, the hip did develop some achiness from the bike ride. I now believe that the hip just won't tolerate repetitve motion with too closed a hip angle (flexing). As an experiment, I started to do some 5 minute sessions of straight-legged jogging since it involves a very open hip angle and little flexing. I also put some very short cranks (152mm instead of 172mm) on my bike and brought the handlebars very high and close so that I'm sitting practically vertical - this is to open up the hip angle and minimize flexing. I did a 30-minute bike ride on the 12th and it was tolerated better than last week, as was the jogging. The yoga classes continue to go very well.
There is a major obvious limitation in my right hip in external rotation. If I sit on a chair with my right ankle crossed on top of my left knee, and let my right knee fall toward the ground - the right knee doesn't fall nearly as far as when this is done with the legs reversed. If I just sit for a minute or two with my right leg crossed like this and relax into the discomfort and try to let that right knee fall further and further, I discover more and more layers of tightness and discomfort. To me, this reveals how much the soft tissues surrounding the hip joint have reprogrammed themselves after the accident in an attempt to protect the joint. Somehow, this must slowly be reversed.
I did a 60-minute easy ride on the 18th and I'm afraid the bursitis/inflammation/stiffness really flared up again two days later. I'm going to put off further attempts at bicycling for a while and work on muscle strengthening in the gym and jogging with fairly straight legs to keep the hip angle open, in addition to the yoga. Perhaps I will be able to slowly increase the jogging to 20-30 minutes and I can get my first meaningful cardiovascular workout in 15 months.
October 4, 2006
The jogging also led to inflammation. I'm going to put off my attempts at cardiovascular activities for the near future and just work on yoga and pilates. I did my first pilates exercise class last night and it should work well with yoga in improving core strength and flexibility. Perhaps the hip needs even more time before cycling or jogging can be pursued.
November 8, 2006
Since things don't seem to be improving with time (the inflammation flared up again last week), I went to see a new physical therapist today who was highly recommended by the yoga teachers in my area. She examined my hip/pelvic alignment and my gait (very messed up) in ways that nobody had previously checked. She believes that the crash caused a significant misalignment of my two hips and resulted in a functional leg length discrepancy, alterations in my gait, and overcompensating (overprotecting) musculature and nerves. There's a tight hip capsule, many weak and tight muscles, and out-of-whack muscular innervation. I've been going for 3 intense, long sessions per week that include some combination of exercises, electrostim (sometimes with solution), ultrasound (sometimes with medication), galvanic ultrasound, electro treatment of trigger points, electro/laser accupuncture, deep tissue work,etc. On days that I don't have treatment, I do about 2 hours of home exercises and stretching that have been assigned. Her approach definitely seems a quantum leap in terms of being more comprehensive, intense, and engaged than any other practitioners to date.
December 12, 2006
For the past year I have been somewhat haunted with the notion of surgically repairing the scar tissue and adhesions. A potential new source of optimism dawned yesterday during my physical therapy session. My therapist was doing some deep tissue massage along the incision scar. Almost out of the blue, she suggested the possibility of having a plastic surgeon open the incision and re-suture each of the tissue layers using absorbable gel sheeting between the layers to prevent adhesions from reforming while healing. This might be the mystery procedure that I've been waiting for, that nobody else previously mentioned. The root of my problem might very well be adhesion between the iliotibial band (ITB) and vastus lateralis (quadriceps) at the site of the incision. I am scheduled to consult with a plastic surgeon in three weeks and continuing with the physical therapy in the meantime.
(postscript: the plastic surgeon told me to stick with an orthopedic surgeon)
December 23, 2006
I am definitely getting strength back into the hip with the 3X/week physical therapy and home exercises. I saw my orthopedist at the Hospital for Special Surgery in New York today. I am going to have him perform corrective surgery in early February - he will open the old incision, remove the scarring, repair a defect (dent) in my quad muscle caused by the old surgery, go up higher into the hip with an arthroscope and clean up the area around the abductor tendon, go into the joint space with the arthroscope and clean up cartilage damage, and finally carefully resuture using a gel compound to prevent additional scarring. In the meantime, I will continue with the therapy/exercises and strengthen my hip further. The hip is tolerating the therapy and exercises well, with just a little baseline soreness - despite the fact that many of the therapy sessions include tissue work that is excruciatingly painful at times. However, long walks (1-2 miles) and swimming still seem to aggravate the hip.
January 15-25, 2007
My continued work with the physical therapist seems to be bearing fruit. The deep tissue work in the gluteal, posterolateral hip, quadriceps and ITB areas is noticeably less painful. I've started using a dense foam cylinder and a 6 inch 1kg rubber ball at home to sit/lie on with my glute/hip region and roll back and forth with body weight - this seems to be really helping and this also is becoming less painful and more pleasurable.
My therapist has identified two additional suspected problem areas, which correlate well with the June MRI report:
1. Scarring of the posterolateral capsule, the ileofemoral ligament to be specific. This would result in a loss of flexibility and difficulty with internal rotation, which is a big problem for me.
2. A bone spur near the origin of the vastus lateralis (quadriceps) muscle, which might be contributing to the difficulty with sustained exercise programs. The spur would be located in the trochanteric region.
I met with the surgeon again and discussed all the problem areas. He should be able to address all of them with the possible exception of the bone spur. He doesn't want to detach any muscles or tendons in order to work on the bone spur at the point and I totally agreed with his assessment.
He has ordered a continuous passive motion machine to mobilize my hip immediately following surgery. I found a Web site which has good information on the types of adhesions that such a device can help prevent. I surely wish my first surgeon had been more aware of these issues. To quote: "this cross-linking can lead to adhesion formation in the soft tissues, stiffness, and the subsequent loss of passive and active motion in the patient." This is exactly what my therapist has been battling to overcome in my hip.
February 11, 2007 - Surgery #3
The surgery was performed Feb.6 in New York and reportedly went well. The minor labral tear was repaired, scarring in the old incision was removed, scarring in the iliotibial band was removed, the noticeable defect in the iliotibial band was repaired, and the inflamed trochanteric bursa was removed. The vastus lateralis (quadriceps) reportedly looked good (palpable defect was actually in the ITB), as did the capsule and other structures. He said the joint itself was in pretty good shape and showed me photos revealing smooth white/pink cartilage. I am wearing a hip brace for a few weeks and using a CPM machine several hours per day as well as a "Game Ready" cryotherapy cold pump for several hours in 30 minute applications. I will probably be on crutches for 2-4 weeks. I feel a bit of soreness from the surgery in several areas of the hip and quadriceps muscle and there is moderate edema in the thigh/knee (I was told this is normal). There is also noticeable "bruising" in several areas, but the surgeon told me that this is just normal staining from post-op blood. I am not on any pain medication. I believe the post-op hip is doing very well.
I wanted to comment on the effect of the anesthetic, especially in light of my experience from the initial surgery back in 7/2005. Knowing that I would be given an epidural, I asked the anesthesiologist to keep any additional sedative to the minimum amount absolutely necessary. I suspect that he ignored my request. Once again, it took about 7 days for me to no longer feel any residual effects of the anesthetic. During a 4 hour period of the night after the surgery, I took 2 percocets. Before taking the percocets, I was out of bed on crutches hopping around the hospital halls. But after the percocets, I went through a 6-hour period of not being able to stand for more than a minute or two without a drastic drop in blood pressure. This was probably due to a combination of the residual effect of the anesthetic, the percocets, and mild hypovolemia (dehydration). The first time I got out of bed early in the morning, I knew I was about to lose consciousness and did so (twice). Gladly, the hospital staff did not make a big deal out of it like my earlier experience 7/2005, and they carried me back to bed and started pumping me full of fluids and tested my blood pressure over the next several hours.
February 20, 2007
The two twenty minute bike trainer sessions are well tolerated, especially in light of my notes above after the 12/30/05 surgery. In the past few days, there's been pronounced stiffness/soreness in the ITB in the lower half of my lateral thigh down to the knee. After several minutes on the bike trainer, the stiffness/soreness is barely noticeable however. I also notice zero subsequent pain, which had been my nemesis for the past 19 months. The ITB soreness has also started to bother me during the night, especially when trying to sleep on my unaffected (left) side.
February 24, 2007
The therapist introduced some resistance exercises (knee/hip extension, ankle pumps) and internal/external rotation (rotational discs). The next day the stiffness/soreness, especially just above the knee and to the outside (lateral) of the knee, was noticeably worse. We backed off on the exercises the next time, but have continued the bike trainer sessions. The surgeon's assistant told me the stiffness/soreness is not unusual and nothing to worry about at this stage. Otherwise, the hip seems to be doing quite well and I've progressed to using only one crutch.
March 2, 2007
The specific stiffness/soreness around the knee started to abate after 4-5 days. The only puffiness left in my leg is above the knee, where there's a little bruising type discoloration undoubtedly caused by surgical blood that has yet to be resorbed. My quads have started to "wake up" and I can take a few tentative steps without leaning too dramatically. Perhaps I'll be able to walk without crutches in about a week. There's still achiness/soreness in several areas of varying qualities, and the therapist has held off on any more exercises other than low resistance cycling.
March 6, 2007
All the puffiness is gone, and my leg muscles are all functioning again. I'm able to walk without limping, and I had progressed to using a single crutch. My therapist thinks my soreness in the ITB and area where my bursa used to be is normal healing. However, yesterday I once again tried some quad strengthening exercises in PT and this aggravated my hip, causing additional soreness in those areas. Other than easy spinning on the bike trainer, I'm going to forego additional exercises for two weeks and for the time being, go back to using 2 crutches. I've been sleeping well for quite some time now - I sleep mostly on my back and sometimes alternate with lying on my left (unaffected) side. I use one weighted pillow by my right foot to help prevent external rotation when I'm lying on my back and one pillow between my knees when I'm lying on my left side.
With this latest aggravation, it's become clear to me that my ITB is going to take longer to recover from the surgery than I imagined. I see the doctor again in ten days and will discuss this.
March 11, 2007
After soft tissue surgery, you're going to feel all kinds of aches and pains of varying quality, intensity and localization. The post op period is a confusing several weeks of not quite knowing if you're getting better or if there's something wrong. The one definite was that the pain I experienced after physical therapy last week was new, more intense, and bad. By taking a break from physical therapy, and religiously using my crutches, some clarity is finally beginning to emerge on all the different aches and pains I've been feeling.
March 16, 2007
I had my follow up post-op visit with my surgeon today. He confirmed what I've been suspecting, that the ITB is going to take longer to recover than I originally thought. He did extensive repair work on my ITB - he had to cut it in order to remove underlying inflamed scar tissue as well as repair the defect in it from previous surgical incisions. He said it is still healing from the surgery, and strengthening work really can't start until after the healing is complete. Inflammation needs to be avoided and he recommended that I take anti-inflammatory medication regularly for now, and to start pool therapy (i.e., physical therapy in a pool). The 20-minute periods of low resistance exercise bike, which were well tolerated during the first 4 weeks, now causes some aggravation so I've stopped. I am still on crutches and will begin pool therapy twice a week.
March 31, 2007
I did three therapy sessions in the pool this week. So far, the hip seems to be tolerating them well. I'm taking Naprosyn regularly and have been icing the hip often during the day and evening and it's sore, but I'm quite hopeful that the pool exercises might get me "over the hump" toward strengthening and losing the crutches. My only regret is that I didn't try pool therapy sooner after this or the previous surgeries.
I'm purposely delaying further attempts at cycling on the trainer and walking without the crutches, to give space for at least two weeks of pool therapy without other activity possibly interfering by causing aggravation. I realize that when I'm walking and using the hip, there are the sensations of strength and of pain, each to some degree. The immediate goal is to get to the point where the hip feels stronger than it feels painful.
I continue to be impressed at what an irritable structure the iliotibial band is and how tricky it is to find and walk that fine line between easy tolerable exercise that can progressively strengthen the hip versus irritating the hip and progressive inflammation.
April 25, 2007
It's been another tough four weeks. After a pool session, I swam 25 yards freestyle with the okay of the therapist. It felt fine at the time, but the hip was aggravated for a week after that. I stopped doing the pool sessions. I started to slowly introduce some walking without crutches. I also decided to start up again with my main physical therapist 3X/week to work on the inflammation as well as strengthening, although I've only had one session at this point. The leg felt good after that session but I made the mistake of doing two minutes of low resistance exercise bike which really aggravated the hip. It seems to be unavoidably aggravated to one extent or another all the time and I'm resigned to that fact. I'd like to get off the crutches entirely in the next week. I did an Iyengar yoga class yesterday and it seemed to go very well, but my body was a bit of a mess this morning and I knew I needed a pelvic adjustment because I had somehow torqued it and I was reminded of the fact everytime I got up from a chair.
May 4, 2007
April 25 ended up being my last day with any use of crutches, so it was 11 weeks total on crutches. On April 30, my therapist introduced some strengthening exercises to my 3X/week sessions. I am seeing good progress on the strengthening and my hip is tolerating it well so far. It's still always a little sore and stiff, but I'm not feeling any new pain after the exercises. I'm also starting to do my strengthening routine at home on a daily basis with therabands. For the first time yesterday, I walked up two flights of stairs. Optimism dawns.
My therapist has forbidden me from engaging in any exercise with repetitive motion until significant strengthening has been demonstrated. In terms of what I've went through over the past 21 months, this makes perfect sense. I'm hoping to be able to try some swimming or biking at the end of the month if all goes well.
May 17, 2007
I had my 3-month postop followup with my surgeon May 11. He tested my hip muscle strength and was both surprised and VERY happy about my progress since the March appointment. He said I should cut back on the Naprosyn, I could slowly begin all activities (bicycling, swimming), and I should expect it to take up to another year(?!) for all hip limitations to resolve.
I've made great gains in the last week in terms of strength and now I'm suddenly going up and down stairs and was able to walk a brisk mile without much subsequent achiness. The hip still has a low level of baseline "soreness" and stiffness. But my activity/exercise has really ramped up in the last couple of weeks. The fact that the achiness never spikes up to a problematic level is a very good sign. I've come to know every subtlety of my hip sensations very well over the past two years.
Another surprising positive sign is that yesterday my therapist intended to do the first session of deep tissue massage on my hip since the surgery. She spent a lot of time on this work about 7 months ago, and it was VERY painful and very obviously needed. However, when she started working on my hip yesterday, it wasn't painful at all and she only worked for a few minutes because it's simply not needed now.
I've also just begun riding the bicycle on the trainer again - I did 20 minutes with a little resistance yesterday. My hip doesn't feel aggravated from it today and I know this would have killed me a few weeks ago.
May 22, 2007
I did a very easy 4-mile bike ride on 5/18 and felt pretty good afterwards. I then did an easy 8-mile bike ride on 5/20. I felt a bit achey the next day and my therapist did some painful massage. It's not feeling so good today and I suspect that once again I have to put off my hope of getting back on the bike soon. I'm going to try some swimming next week down in Florida and we'll see how that goes. It's possible that I may need to start over again and just do some yoga for a few weeks and forego all repetitive motion.
June 3, 2007
I swam 50 yards freestyle last Tuesday and 100 yards on Thursday. Any residual soreness was minimal, and this was very encouraging. Last week my therapist suggested that I ride my bike once per week for whatever distance/effort I wished as long as there was no pain at all. This would allow a week between rides to recuperate with the help of therapy. I rode 16 miles yesterday with moderate effort. I was a bit sore afterward (no surprise) and a bit apprehensive. But it's not feeling that bad today, and this is again very encouraging. I have been diligent with my daily exercise routine, and the hip strengthening seems to be paying off.
June 11, 2007
I got the green light from the therapist to ride again, and did 17 miles 4 days ago. I felt virtually NO soreness afterward and this was a very happy surprise. I did 20 miles two days later and although my butt ached toward the end, there again was no complaints from my hip. I'm 4 months since the last surgery and suddenly (not gradually) everything has turned around in the last week, and is looking very positive toward resuming physical activity at a high level. At the same time, my hip suddenly feels more natural/normal in everyday movements.
June 18, 2007
I'm continuing to do 15-20 mile rides every 2-3 days. Sometimes the hip is a little sore, but no big deal so far. The only thing that's really bothering me for a few days after rides is my neck, which I assume needs to regain some strength. I did one fairly easy club ride and quickly realized that I'm not up for hard efforts yet and best to put those off till next season. An easy half or metric century (solo) by the end of the season is a more realistic goal. The orthopedists have consistently said that it takes twelve months to fully come back from injury/surgery like this, and now I'm finally understanding.
June 29, 2007
The riding continues to go well. I have to be careful of not pushing too hard with too low a pedal cadence or my knees really feel sore afterward. The muscles and lungs are willing/able but the knee tendons need a period of easy miles to get strong. I managed 250 miles of riding in my first month back and I expect this to continue to increase for the next few months. I hope to be doing occasional 50-60 mile rides in August/September.
I did my first yoga class in about 6 weeks and was amazed at how much better the hip felt. Sitting cross-legged on the mat was markedly improved as is standing straight up. I should also mention that I've been able to discontinue physical therapy.
September 29, 2007
I've met my goals back on the bike but I just wanted to mention that my pelvis/SI joint continues to need adjustment every 1-3 weeks by my physical therapist. The symptoms of alignment issues for me are mainly soreness in my hip and perhaps a feeling of a slight discrepancy in leg length from side to side. My therapist is quite expert at getting it back in alignment. There's obviously muscle imbalance or weakness and I need to give this some attention.
October 16, 2007
I've stopped bicycling to give full attention to the muscle imbalance and have started twice weekly Pilates sessions focusing on my legs. During the first session, it was very apparent that I need to retrain my right hip for proper motion - the nerves/muscles had adapted to the injury/recovery in ways that needed to be unlearned.
November 2, 2007
I stopped the Pilates sessions to give full attention to the SI joint instability. I needed to gain awareness of my SI joint's tendency to "go out" on a frequent basis and gain independence from my need to go to my physical therapist to get my SI joint "back in".
I found a great resource on SI Joint problems at www.calindra.com and tried some of the exercises. I had an epiphany soon after - I realized that I was suddenly experiencing absolutely no discomfort when I did some of my routine stretches to the extreme ranges of motion. This convinced me that the fundamental short term problem was the SI Joint. Unfortunately, in my exuberance of feeling so good, I went out for a short gentle jog and messed it up again and couldn't get rid of the discomfort.
A few days later, I spent 3 hours with a yoga therapist who generously shared her experience overcoming SI joint problems. As a result of what she showed me, the exercises she prescribed, and DonTigny's exercises from kalindra.com, I can now do daily stretches and exercises and consistently know when my SI joint is out and get it back in. She also showed me that I can lie down and sense the (in)equality in my leg length myself and objectively see the correction after the exercises (and the felt "pop"). I've held off on any aerobic exercising and the hip is once again feeling very good. So I'm now laying a baseline of health in the SI Joint and hip and will eventually try to slowly add some strengthening and aerobic exercise to the mix. I am getting quite astute at feeling immediately when the SI Joint starts going out, and that's really what I needed.
December 28, 2007
I still haven't been able to resume a consistent program of exercise that involves the affected hip. The hip gets sore and there's significant SI involvement. I'm still searching for a rehab solution.
March 2008
On the advice of my NYC surgeon's assistant, I attempted to begin a regular program of strengthening and stretching of the hip. My hip soon got very sore from the strengthening but I continued with the yoga. I noticed that I started having frequent attacks of lumbosacral (lower back) stiffness and pain and that these attacks were getting worse and worse. I stopped all activity and went to see a different physical therapist to seek relief from my acute back problem. He quickly surmised that the cause of my back problem was unresolved hip issues. He pointed out that my right glutes were significantly atrophied and my ITB was tight. He started with some myofascial release work on my piriformis and glute medius muscles which really seemed to need it. I'm also doing a lot of stretching. Soon I will begin a very gradual program of hip strengthening, focusing on the extensors and abductors.
I also went back down to NYC and saw my surgeon again and his favorite physical therapist for a consultation. It honestly didn't prove that helpful with nothing really new being heard.
April 2008
During a two week vacation break from physical therapy, I was able to walk/hike several miles each day that included a few fairly intense up/down hikes in the desert. The hip did really well. I returned to physical therapy right after I got back. The therapist, for whatever reason, suggested I try several new strengthening exercises during my session. The next day my hip started to ache and over the next two weeks, the hip slowly got progressively worse. In hindsight, I was probably a little overconfident after the hiking during my vacation and my therapist was a bit reckless and we did way too much too fast. I've stopped physical therapy, and I see no point in going back. I stretch my hip religiously every day and I am just waiting for it to return to baseline. It might take a month to do that and this is really slow going. After the hip settles back down, I'll try some easy bicycling. If that doesn't work, I'll stick to hiking.
May 2008
As expected, it took a full four weeks for the hip to settle down. On the advice of a Naturopath, I've started taking a proteolytic enzyme (18 tablets daily of Wobenzym-N). There's a huge amount of anecdotal information on Wobenzym successfully treating injuries, inflammation, scar tissue, etc. The Naturopath also insisted that I ramp up the bicycling much more slowly than I did last June and avoid club rides. I've done very easy 4, 6, and 8-mile rides with two rest days between recently and so far so good.
June/July 2008
I continue to make slow progress. I started June doing easy 10-15 mile rides as well as a fair amount of rigorous hiking. The hip seemed to tolerate the hiking better than the bicycling. I found it hard to determine whether the achiness in my hip 1-2 days after bicycling was getting better or not, so I began to keep a detailed daily log on how the hip felt. I found this VERY helpful because I learned that a lot of the achiness was happening routinely and wasn't cause for concern. By the third week of June I was doing 25-mile rides. However, I still need to take at least 2-3 days off between 25-mile rides to avoid aggravation.
My recuperation is decidedly different that I expected in one specific respect. I expected my hip pain and discomfort to decrease slowly but consistently until my hip felt more or less "normal." I now realize that the recovery is a lot less about feeling and a lot more about function. Even though my hip hasn't been feeling much better lately, I am hopeful that functionally it is getting more and more capable of sustained exercise. Again, keeping the daily log has helped me realize this. Now that I'm doing some regular substantial exercise, the hip "feels" much stiffer. I am diligently stretching it twice daily now and although I've maintained very good range of motion, I can definitely feel the stiffness when I stretch it deeply in certain directions.
September/October 2008
I had an MRI of my hip. It showed that there has been some progressive arthritic degeneration in the hip cartilage evident since the surgery 19 months previously. This was a bit of a shocker since after the surgery I was told that the cartilage looked good. My surgeon things these changes are responsible for my difficulty in resuming a high level of activity. He mentioned that cartilage issues also can manifest as inflammation in the surrounding musculature. He suggested trying other forms of activity to alternate with bicycling, such as swimming. He also said that Active Release Therapy might be helpful (can you say "deja vu all over again"?).
At first, I found this new diagnosis a bit strange because I've had pretty much the same issues for the past 3 years, not just since these changes showed up on the MRI. After mulling it over for two weeks, I am beginning to accept it as a possibility. I can't deny that I was able to put in significantly more miles last year on the bike than this year. But I've made great progress since April/May of this year. So I'll continue and take the cycling as far as it will go. I've started to educate myself about hip resurfacing, but have little interest in going under the knife for a major hip operation again. I did speak with Dr. Su's office - he's one of the leading hip resurfacing surgeons in the USA. They looked at my MRI and said I was definitely a candidate for the procedure and encouraged me to go as far as I can using anti-inflammatories (Naproxen) on a regular basis. They discounted the possibility of liver/kidney issues from the Naproxen as long as my stomach can tolerate it. So I'm taking Naproxen regularly now, and I'm experimenting with shorter/easier rides on a more frequent basis.
For what it's worth, I've cut way back on my stretching and I actually believe this has helped a little bit. Besides a few McKenzie back stretches, I'm just doing hamstring stretches and a little "hips-to-each-side with bent knees" to pop/mobilize my lumbar spine and SI joint. I still feel just as strongly that mobilizing the SI joint is critical.
November 2008
I made a trip out to Syracuse NY and was seen by Dr. Michael Clarke, another one of the leading hip resurfacing surgeons in the USA. He is fairly certain that my exercise intolerance is being caused by some degeneration of my hip cartilage and this was brought on by the hip fracture. He performed a cortisone injection into the hip joint, mainly for diagnostic purposes. It didn't seem to help. The next step with him would be a hip arthroscopy, so that he can see the condition of the joint surface up close to determine whether a resurfacing is indicated.
December 2008
I consulted another orthopedist and read widely about hip resurfacing and it seems that my hip degeneration isn't nearly as bad as would be expected for a resurfacing patient. So I'm not going to proceed down that route at this time. I've joined the local "Y" and will attempt to slowly build up my swimming endurance and see if I can tolerate that as a regular exercise regimen. I am very aware that I have lost so much strength in my leg muscles and this isn't helping my hip at all, so I hope to reverse that.
January 2009
I'm swimming (freestyle crawl) every other day for about 30 minutes. Even though I'm trying to minimize my kicking, the hip still feels a bit sore. So I'm living with a baseline level of soreness and often take Naproxen, but I'm still maintaining the every-other-day swimming routine. I'm already come far in my swimming technique - at first I couldn't swim more than a lap or two without being totally out of breath. But I've had a few lessons and am doing much better now. I haven't gone near a bike since Thanksgiving.
February 2009
I've had a few sessions with a chiropractor who specializes in applied and clinical kinesiology. It seems that there are still ongoing structural alignment issues in the pelvis/SI that are affecting the hip's functionality. There also seem to be some significant adhesions, particularly in the area of the ITB/Tensor Fascia Latae/Vastus Lateralis. This was also called out on my Sept '08 MRI. She did some deep fascial release work on the adhesions and the extreme pain was deja vu all over again.
March 2009
The chiropractic work seems to be helping. I've been swimming a few times a week and I've just started with some occasional short easy bike rides. I realized that I haven't take any ibuprofen in a few months. So there's more optimism on my part that the orthopedists were wrong in simply declaring me a degenerated joint cartilage fait accompli based on my September MRI. This included my surgeon, who in Feb '07 sought to repair my ITB adhesions and now seemed to ignore my September MRI finding that those significant ITB adhesions still existed. I unquestionably still have significant soft tissue issues involving some combination of my ITB, vastus lateralis, tensor fascia latae and piriformis. Fixing those soft tissue issues seems to require mounting a grail-quest type effort considering the state and approach of our modern medical system.
May 2009
I started playing some golf in an attempt to find an activity that would be easy on my hip. After several weeks I began experiencing extreme stiffness in my left mid-back which kept coming back. My new chiropractor told me it's due to weakness and instability in my right hip and right foot. I will be addressing the foot issues with some new orthotics which he feels will really help my hip. He gave me a convincing demonstration of this by doing a tape job on my right foot (heel and ankle mostly) and I was amazed at how my right hip suddenly felt unburdened. He is also having me do some hip exercises, especially to strengthen my gluteus medius. I continue to swim occasionally when my back isn't bothering me. Walking and swimming are about the only activities that my hip can mostly tolerate.
June 2009
I've switched my aerobic workout from swimming to vigorous treadmill walking, varying incline from 8-12% and speed 3.3 - 4mph. I like being able to monitor my heartrate (maintaining ~150bpm), listening to music, and avoiding chlorine. Paying close attention to gait and posture, I think the weight bearing is helping strengthen/balance my hip muscles in ways that swimming or cycling don't touch. I've also started doing regular flexibility/strengthening exercises with an Egoscue workout DVD. The Egoscue method is incredible - it has significant hip and back benefits and helps to restore natural balance and strength in the body.
I've been totally off the bike for over 2 months now and my hip is feeling the best it has since the accident.
August 2009
I traveled to Boston to see a sports medicine physiatrist (MD). After studying my history and examining me, he thought that my problem didn't involve the joint cartilage and suspected a torn tendon that never healed. I am going to follow up later this month with an ultrasound exam to look for the tendon tear as well as platelet rich plasma (PRP) injections to stimulate healing.
update (two weeks later): I purposely aggravated my hip by going for two bike rides. The physiatrist had marked my leg in the spot that overlied the suspected tendon tear. He asked me to aggravate the hip to confirm the spot as the focus of the pain. However I didn't find much correlation between my pain and that spot. Before proceeding with the PRP injection(s), I've decided to first go back to Dr. Clarke with an aggravated hip and repeat the diagnostic injection into the joint to rule in/out the joint as the source of pain (rather than soft tissue). If that test proves negative, I intend to aggressively pursue expert PRP injection therapy.
March 2010
Status hasn't changed - I am doing spinning classes and starting to ride on the road. I anticipate that the hip pain will eventually become constant and I will then return to Dr. Clarke for the diagnostic injection.
April 2010
After about 3 weeks of spinning classes and riding, the hip pain came on in the usual way. It's clear that I can't ride more than maybe once per week. The pain is such that I don't think any doctor is going to localize the source and even if it was my joint, I'm not going to consider more surgery at this point. I'm going to back off from riding as I did last year and focus my attention on trying to develop a barely decent golf game.
May 2010
At this point, I'm pretty much throwing in the towel. There's just too much misery that accompanies an aggravated hip when I keep testing it by bicycling. Golf and hiking will have to fulfill my athletic ambitions. I've decided against pursuing further medical diagnosis or surgery at the hands of always-overly-optimistic physicians.
August - September 2010
Okay, I guess I picked up the towel again. I was seeing a local orthopedist about a different issue and the conversation came around to my hip and I asked him what he thought about me seeing a physiatrist to help with diagnosis. He thought it a good idea and referred me to a physiatrist in their group. I saw him today and I just wish I saw him 3 years earlier (why didn't any of the million orthopedists I've seen ever suggest this?). After reviewing my history, and doing some quick tests he was convinced almost immediately that my problem was NOT my joint ("you'd never be able to effortlessly hop up and down on your affected leg if it was your joint - this is easily ruled out by this simple test") but inflammation caused by the scar tissue between my ITB and vastus lateralis muscle which secondarily is inflaming a bursa in the area. He said the scar tissue is clearly seen on the MRI from '08.
He suggested trying prolotherapy (local injections of platelet rich plasma gel) and arranged for me to be seen the next day by the sports medicine doc in the group that is just starting to do the injections. Wow, what a quick turn-around. I can't help but continue to look back with frustration at the mis-diagnosis by my surgeon in October '08 after the MRI.
So I started riding again, in part to purposely aggravate my hip again to try and localize the areas of pain. For the first 6 weeks, I experienced predominantly stiffness rather than pain. From week 6 onwards, soreness started becoming a bigger component. This progressive pattern is typical of what I experienced in the past. The stiffness and soreness is diffuse and impossible to localize.
So now I'm patiently waiting for the PRP procedure to be performed on my hip. I'm also relieved to learn that the treatment can be applied in a large general area around the hip and it's not necessary that a small anatomical target be identified.
October 2010
The riding was going well although I sensed an underlying progressive stiffness in the hip. Then on one ride, I sensed that something was wrong - getting up out of the saddle and I felt lower back pain/stiffness and I instantly thought of the lower back/SI problems I've had in the past. It seems the exact same progression occurred as back in late '07-'08. I guess it's time to once again to put down the bike and try to address possible underlying muscle imbalance.
February 2011
The PRP injections never happened - the Orthopedic group still needs to lay the groundwork to offer this new procedure. I did spinning classes for several weeks and then the hip aggravation progressed to the point that I had to stop. It's the same cycle repeating itself. I'm not hopeful at this point.
June 2011
I'm on the bike again, but I'm typically giving myself 3 off days between rides, so only riding 1 - 2 times per week and about 30 miles per ride. I'm also using a foam roller for a minute or two on a daily basis to keep the ITB from tightening too much. So the combination of very modest mileage (i.e., lowered expectations) and foam roller is keeping me riding.
September 2011
The Orthopedic Group finally came through and I had the PRP injection Sept 15. The injection targetted an area of soft tissue around the trochanter, using ultrasound for guidance. It was not a painful procedure at all and the hip is just slightly sore the next day. I was told to not exercise the hip for one week and then we'll take it from there.
December 2011
The injection seems to have helped although time will tell. I'm trying to maintain a twice weekly indoor cycling workout regimen.
March/April 2012
Unfortunately, things got progressively worse and I'm once again sidelined with hip and SI joint issues and grasping at straws in order to somehow get my hip issue diagnosed. I saw a new local orthopedist who seemed quite competent but essentially just scratched his head. I'm going to stay off the bike indefinitely. I've started wearing an SI belt full-time and I like the added stability to the hip/pelvis. Hiking the local mountains has become my main physical pursuit.
August 2012
I've been off the bike since March. But I've been able to keep up a consistent routine involving rigorous hiking in the local mountains. Once or twice a week I've been doing summit hikes of 6-10+ miles with up to 2000ft elevation gain. There is some stiffness/soreness but it hasn't progressed or side-lined me.
January 2014
I'm still off the bike and doing rigorous hiking. I've hiked about 130 mountain summits since putting down the bike in March 2012, including hiking throughout last winter. I've experienced no progressive hip soreness from the hiking. In the winter I go to the gym and do either an elliptical or inclined treadmill workout. Even at only two workouts per week, the hip can get sore at times.
Summer 2014
I went a little too hard in June - 8 mile hikes on successive days - and the hip went into an aggravated state for the first time in a long time. I had almost forgotten what this felt like and how annoying it is. Even though the pain might only be a 2 or 3, it is very annoying and not something I want to live with for long. There's definitely a "threshold" effect - once the threshold is exceeded and the hip becomes aggravated, it can take a few weeks or even months for the aggravation to resolve, even with inactivity. This is why I went into a period of just playing golf a few years ago.
I'm happy to say I was back on the trail after a few weeks of resting the hip and once again hiking quite strong in July.
Summary of what I learned:
1. Sports/traumatic hip injuries are often accompanied by soft tissue injuries which are more difficult to diagnose and may prove more difficult to deal with than bone/joint injuries and often take years to heal.
2. The effects of traumatic orthopedic surgery on the soft tissue can be more detrimental to patient progress and recovery than the issue resolved by the procedure itself. It is important to mobilize the hip immediately following surgery to minimize soft tissue problems. This was regretably NOT done for me after my initial hip fracture surgery.
3. Orthopedists are often at a loss at diagnosing and directing the treatment of soft tissue injuries, even those resulting from their own surgical intervention. Many hip orthopedists are not expert at treating sports injuries. Physiatrists (physical medicine MDs) can be your best bet at pinpointing the source of orthopedic problems.
4. Essentially EVERY physician is overly optimistic about outcomes - unfortunately, you must take their predictions with a grain of salt.
5. Physical Therapists vary enormously in their experience and ability to treat complex soft tissue issues. In addition, you need to find a therapist that will devote a lot of time to you - your visits should be measured in hours, and not minutes. You should be given a daily home exercise and stretching routine.
6. If your hip can't tolerate the strengthening exercises in the therapist's office, don't hesitate to find a therapist who's expert in pool therapy and start working with him/her in a pool. You won't believe how beneficial this can be, especially in the beginning while you're still on crutches. It's often hard for the hip to make the transition to suddenly exercising after surgery and resting for several weeks, so go slow and start in the pool.
7. It's crucial to your recovery that you work VERY hard at strengthening the hip. It's difficult to comprehend to what degree the muscles and connective tissues are weakened by surgery and trauma - a MUCH greater degree than inactivity itself. Do not equate the mere absence of pain with recovery. Functionality along with some degree of soreness is VASTLY preferable to a degree of comfort resulting from rest/inactivity. You need to go through several months of some level of soreness while regaining strength and functionality. This was a very important, yet difficult lesson learned through months and months of trial and error without guidance.
8. In parallel with your efforts at strengthening the hip, should be a daily routine of extensive hip stretching. This should continue on a daily basis even after you regain total range of motion in the hip. Along with the hip stretches, be sure to include stretching of the piriformis, ITB, and hamstrings along with stretches that mobilize the SI joint.
9. Patience, patience, patience is absolutely necessary when recovering from soft tissue injuries.
10. After significant trauma and a lengthy period of diminished activity in the hip, special attention needs to be given to relearning proper hip motion in conjunction with strengthening. Strengthening alone will leave your hip's muscles and nerves operating with abnormal compensation that needs to be unlearned. This compensation won't go away on its own, even though your hip seems to have regained its strength.
11. After a hip trauma such as this, there is a high likelihood of SI Joint issues due to the side-to-side imbalance that will ensue in the hip/pelvic/lower back region. Attention much be given to diagnosing the issue, mobilizing the SI Joint through flexibility training, and strengthening the structures to stabilize the SI Joint. There's an excellent discussion of the SI joint mechanics by Neil Chasan, PT
12. In choosing an orthopedist or therapist, you can't be too careful in finding out as much as possible - ask everyone you run into for their input on hip orthopedists or therapists in your area. Get on internet sports and sports injury forums and ask questions and do research. Don't hesitate to see several practitioners until you know you're under excellent care. Really good therapists and orthopedists are really hard to find (really), but they ARE out there, and they ARE really good.
13. MRI machines vary greatly in their image quality and you need a radiologist who specializes in bone/joint issues. Even so, it is extremely hard to get a diagnosis of soft tissue issues on an MRI. You need to exercise just as much care in selecting your imaging center and radiologist. If you possibly can, go to the Hospital for Special Surgery in New York and have Hollis Potter conduct/read the exam.
14. Don't hesitate to go outside your local area for health care if you must, in order to find excellent practitioners. Along the way, I consulted with orthopedists in Colorado, Tennessee and New York City as well as my local area. I travelled 150 miles roundtrip twice a week for Active Release Technique sessions.
15. You need to be quite disciplined about eating habits due to almost total loss of all physical activity. I was able to maintain my pre-fracture weight throughout, but it meant eating A LOT less.
16. Some people (me) are sensitive to the effects of anesthesia. It seems difficult to convince anesthesiologists to lower the dose. For sensitive individuals, it's probably best to avoid all opiate pain medication, especially for 72-hours post-op. I can routinely feel the effects of general anesthesia for a full week after surgery.
17. Proper foot support (orthotics, etc) is important in order to regain proper side-to-side balance after hip injury. Your body will go through various stages of compensation while recovering and having any foot or knee issues may stall the recovery in a compensated/unbalanced state.
18. Ride with adequate hip padding/protection to avoid ever having to go through this. I've experimented with various padding solutions since my accident and the following is what I currently use - this combo is actually not bulky, quite comfortable on both recumbent and racing bikes, provides excellent impact/abrasion protection, and moves well with your legs:
inner layer: lightweight cycling shorts with unpadded chamois (absorb sweat)
middle layer: McDavid 755T Hexpad Football Shorts (only hip pads used)
outerlayer: Fox Launch shorts (one size larger)
Links to other hip fracture recovery journals:
Steve Martin's story
Links to other hip injury information:
Hip Patient Education Articles
Hip Resurfacing Info Center
Coming Back from a Broken Hip
My long road to recovery from hip fracture surgery and soft tissue injuries after a bicycling accident
Saturday, July 23, 2005
On July 23, 2005 my right hip was fractured during an 80-mile bicycle ride on the roads of the Adirondack mountains. The cyclist in front of me hit something in the road, lost control of his bike and slid into me from the left side, taking both my wheels out and causing my right side to slam into the pavement. I was taken for a long ambulance ride to the nearest hospital where I was admitted after x-rays indicated a non-displaced intertrochanteric fracture of the right hip. The fracture was surgically repaired the following day by installing a compression hip screw and plate (see pictures below), anchored by 3 screws into my femur.
I've found very little information on what to expect in the long recovery from this injury, either from my doctors or from the internet. My naive expectations of a straightforward recovery over the course of a few months were not realized, so I thought I'd post a detailed account of my experience for the benefit of others who unfortunately experience a similar mishap. Ken Kifer posted the only other account I could find that was truly very helpful. At the bottom of this page, after the chronology, is a summary of what I learned through this ordeal. It's probably worth mentioning that I'm middle-aged (although "young" for my age), athletic, and fairly svelte (5'10" 140lbs).
Hospitalization:
After the accident, I spent 6 days in the acute care hospital and another 6 days in a rehab hospital. Before they performed the surgery, suffice it to say that any movement of the bad leg was absolutely excruciating. They had me out of bed on crutches the day after surgery, and I managed fairly well. However, I had a few fainting spells in the acute hospital - they occurred soon after starting a walking episode and were accompanied by very low BP. This was almost certainly due to blood loss in the accident and surgery combined with lingering effects of the general anesthetic and pain medication, although the hospital insisted on putting me through every diagnostic test imaginable (2CAT scans, EEG, etc).
 On the left is a photo of the compression hip screw and plate that was implanted in my right hip. The lower part of the plate that runs snug along the femur is secured by 3 screws (not shown) through the femur. (See further below for an additional photo of the hardware with screws.)
On the left is a photo of the compression hip screw and plate that was implanted in my right hip. The lower part of the plate that runs snug along the femur is secured by 3 screws (not shown) through the femur. (See further below for an additional photo of the hardware with screws.)I was on a morphine pump for pain for the first 48 hours and then on oral percocet. I didn't use much of it because I wasn't really in that much pain after the surgery. One side note is that the general anesthetic combined with the opiate pain medication had a marked effect of depressing smooth muscle function - in other words, your eliminative functions really slow down. Morphine also have a strange nightmarish effect on your dreams. I did have a fair amount of muscle spasms in the hip, especially during walks on crutches. I was put on flexoril and this calmed down the spasms. After about a week or so, the spasms were gone.
I figured out how to grab my right leg with my good left leg, cradling it with the left foot. This is an important skill, because it took more than a month for me to be able to swing my right leg down from the bed using the muscles in the right leg. It was also really tough at first to put my right shoe on and to put pants on.
Physical therapy began in the hospital soon after the surgery. The therapy routine became much more serious when I got to the rehab hospital. There's a clear intention to get you independent so you can go home. It's a combination of strengthening, stretching, and practice simulating household environment (stairs, shower, etc).
What was especially disconcerting was the almost total inability to bend my knee. My quads and leg felt as stiff as a board. This was to be my nemesis for the coming months. From the little I could find out, the degree of stiffness in knee flexure that I experienced was quite unusual. It was later suggested that the knee stiffness was probably a result of the trauma suffered from the impact to the soft tissues of my leg and not the hip fracture itself.
Release:
On August 3, I was released from the Rehab hospital. Before release, they removed the staples from the surgical incision and applied steri-strips. This is normally done at 14 days post-op and in retrospect, it was a mistake to remove them a few days early because the wound wasn't 100% closed. They also trained me to give myself injections of anti-coagulant, which would be continued up until 4 weeks post-op. This was the only medication I was taking.
After returning home, it suddenly became apparent how much effort it took to get around the house and do all the little things when you're living alone. On August 4, I became aware of increasing edema/swelling in my leg. By the evening, even my ankle lost all definition and I was worried about the possibility of infection. I spent 5 hours in the ER waiting for a doctor to look at me and tell me to go home. In retrospect, I should have been wearing the compression stocking on the bad leg and staying off the leg a lot more at this early stage. After a night in bed, the swelling had subsided quite a bit.
On August 5, I went to stay with my sister for a week. I really wasn't ready to go it alone and the extra week of taking it easy was exactly what was needed. During this time, I religiously performed the exercises prescribed by the rehab hospital PT. The knee remained very stiff. After I returned home the next week, I discovered that I had no trouble driving. I started physical therapy sessions 2-3X per week.
Around the 3rd or 4th week I learned a trick to help with sleeping. Up until then I was sleeping exclusively on my back. The trick is to use a second pillow as a prop. When sleeping on the unaffected side, put the pillow between your knees. When sleeping on the affected side, put the pillow under your hip. And eventually I started to also use the 2nd pillow when sleeping on my back, placing it under my knee.
Physical Therapy:
The main focus was to regain knee flexibility. At first the prime exercise was the "wall slide." I would lay on my back on a table pushed against the wall. I placed my foot on the wall with my upper thigh perpendicular to the table and try to slide my foot down the wall and flex my knee more and more. The therapist would come over after about 10 minutes and assist the flexure (ouch). If I could attain about 120 deg of flexure, I could advance to the stationary bicycle. At first on the bike, I had to keep the seat quite high with my heel on the pedal to minimize knee flexure. The first few pedal strokes were fairly painful on the upstroke of the bad leg. I would do about 10 minutes of easy pedaling. After a couple of weeks, the therapist added another regimen of stretching between the wall slides and bicycle. I would lay prone on the table and he would flex my knee from the back and push my heel toward my butt. New horizons of pain were continually uncovered.
There were both noticeable steps forward and backward during my physical therapy. As I write now, I am in the 5th week of therapy. I have had two "bad" sessions, where I was in pain afterward, my knee flexion ability took a few days to recover, and I had to take a few days off from therapy. I had one "aha" in therapy Sept.8, where my muscles seemed to wake up and I could suddenly walk unaided with hardly a limp. This was followed by 3 days of walking without any crutch, including stairs. I even managed two easy bike rides 9/10 and 9/11. Unfortunately, one of the bad sessions immediately followed and I regressed to needing the crutch after my quads seemed to significantly weaken due to pain.
Week 6: I continue to be amazed at how quickly the stiffness in the knee and quads return after stretching them. The stiffness is really felt during the stretching as well. After my knee reaches about 90 deg, it is stiff, stiff, stiff. I can continue to push it past 90 degrees - it just becomes increasingly painful. So during the therapy sessions, it is a test of how much pain I can endure translating into how far we're gonna get the knee stretched today. The last session we just went too far and I knew it immediately after I got off the table - the leg hurt, and I was limping.
Around the 5th week post-op, the internal swelling must have subsided because I was suddenly much more aware of the hardware (plate) inside my leg. I started feeling a continual pressure and irritation, as if there was something in my pants pocket. The irritation seems aggravated by a lot of activity. When I walk, there is a constant feeling of slight irritation over the hip plate. The orthopedist says it will probably eventually subside, but if it doesn't, the hardware can be removed. 8 weeks post-op and the orthopedist says I'm doing fine and that it will take 6-12 months for the leg to feel almost normal.
Week 7: In the crash, the bike fared much better than I did. The front wheel was taco'd beyond repair, the bar tape was shredded and the STI levers were badly scratched. I had a new front wheel built, retaped the bars, replaced my helmet and gloves and gingerly ventured out on a 7 mile slow, flat bike ride. There was quite a bit of discomfort on every upstroke of the right leg for the first 10-15 minutes, but otherwise everything was fine. I went out again the next day and the following weekend as well. On my 4th ride of 14 miles, the discomfort was markedly reduced and I started to give just a little bit of effort beyond merely spinning slowly. Afterwards, I realized that my right leg was starting to feel like a leg again. The modest exercise seemed very beneficial. What discomfort there was during the ride, was more in the knees rather than the quads.
Week 8: Now at the 8 week mark, it seems that after a knee flexing session, the stiffness doesn't return so fast or so completely. And when I start a knee flexing session, I get to the 120-130 degree flex much more quickly, without taking 10-15 minutes to work up to it.
There was a pronounced bump in the contour of my hip, caused by the hardware underneath. I was resigned to this as a slight permanent deformity. After 8 weeks, I suddenly realized that the bump had almost completely disappeared, much to my relief.
Week 9: I realized something else about physical therapy. The agressive stretching session is followed by a few days of sore muscles/hipjoint. This soreness is also experienced as weakness (limping) - the body is naturally defensive about the soreness & stress on the muscles/tendons/joints and you feel weak. This week the therapist was able to bend my knee back to within 2 finger widths of my butt, so the flexibility is coming along. For some time afterwards, the area on my leg directly superior and superior/lateral to the knee cap was very sore. In addition to the hip flexors, extendors, abductors, and adductors, I've also added the internal rotators to the daily strengthening exercises.
Week 10 (early October): I went through another sore/painful few days after the last therapy session and after doing a 20-mile bike ride. I saw the surgeon again, who was very happy with the progress. He suggested stopping the physical therapy for a few weeks and see how it goes. He wasn't concerned with recapturing the last few percent of range-of-motion on the knee and was happy I could bike again without discomfort. When I told him that there was irritation over the plate whenever I walked for any distance, he said that we might have to consider removing the plate in another 3-6 months.
November 23, 2005
Since my week 10 posting, the inflammation in my hip centered around the hardware gradually increased to the point where I ceased all exercise activity completely and had to go back on crutches a few times to take the weight off the leg. I received anti-inflammatory injections into the hip to try and tame the inflammation around the hardware. This was a good faith effort by my surgeon to avoid surgical removal of the hardware. He intimated that he would consider removing the hardware in January or February if the injections didn't help. They didn't and my limp slowly got worse.
December 30, 2005 - Surgery #2
I had in-patient surgery to remove the hardware and stayed in the hospital for 24 hours. The surgeon put a drainage tube up into the femoral neck that came out of my leg into a bag. This was removed when I was discharged the next
 day. I arranged to receive the hardware that was removed. The surgeon told me that they had to chip away bone that had already started to grow around the hardware in order to remove it.
day. I arranged to receive the hardware that was removed. The surgeon told me that they had to chip away bone that had already started to grow around the hardware in order to remove it.I was able to get around well enough the day after surgery so that I could fend for myself at home. I took it easy for a week at home and then returned to work. It's now 3 weeks later and I'm still feeling a fair amount of pain and soreness. I started to walk a bit without crutches about 2-1/2 weeks after surgery. But I've already aggravated the pain by some gentle cycling on a trainer and it was quite painful for several days after. There was a sizeable hematoma from the surgery and it's now smaller but the area is still swollen after 3 weeks and causing some discomfort. Sleep is a bit challenging because every night the hip starts bothering me after a few hours of sleep. I spend the rest of the night constantly changing positions between sleeping on my back and on my left side, and use a second pillow under my knees or between my knees.
It will take a few months for the holes in my femur to fill in that were left by the hardware, so strenuous cycling will have to wait till the spring at least.
The photo shows the actual removed hardware in the proper orientation as it was in my leg. The material is either stainless steel or titanium and it weighed a hefty 6 oz. I'm VERY glad that it's out of my leg now.
January 27, 2006
It's now 4 weeks after the removal surgery and I've gone back on crutches in an effort to give the hip the best chance of recovery. It still feels quite aggravated from the 15 minutes of easy trainer cycling I did five days ago.
On the advice of my surgeon, I began physical therapy again on Feb 8. I'm getting iontophoresis (electrical current drives anti-inflammatory medication into the tissues) as well as hot/cold, stretching, ultrasound, massage, and some exercises. The hip still can't take much exercise without being aggravated for a few days afterward.
February 23, 2006
It now appears that the hip still needs more time (rest) before beginning any exercise. It's eight weeks after hardware removal surgery and seven months since the accident. It's hard to accept that an injury could need this much time, but evidently it does. I honestly haven't experienced any improvement as a result of the physical therapy begun two weeks ago. In fact, it seems to have only aggravated the leg. I stopped the physical therapy.
March 9, 2006
I tried 5 minutes of very easy spinning on my trainer and once again it greatly aggravated my hip. It's now 10 weeks since hardware removal. I went in and saw my local orthopedist, trying to find out why the hip is so intolerant of exercise. He told me what I'm experiencing is normal and it's just too soon after the hardware removal surgery. He said I probably will need another 3 months (gulp) before riding much and 6 months to really heal completely. He also warned that I may always have a little pain in the hip in the future. He also said that the fact that the incision scar is still red indicates there's still a lot of inflammation/rebuilding going on. When the scar turns white, that will be a sign that healing has progressed (?!).
April 3, 2006
My condition is still about the same - slight exercise results in ~5 days of mild-moderate aggravation. I visited my GP and we discussed the fact that these injuries normally take about 12 months to heal. But what if, I conjectured, after 12 months the hip still hurts and then we look and find another underlying injury? My GP concurred and suggested we go ahead and get an MRI taken to rule out additional injury. The resulting MRI report indicated that there's still a fracture, which caused some confusion. My surgeon sent the MRI to be re-read in hope of determining whether it's the original fracture that is still healing or whether there might be a new stress fracture. While I wait for the news, the surgeon has put me back on crutches to unweight the hip. He was also concerned because I had a pronounced limp due to aggravation from an easy 1 mile hike three days earlier.
Okay, ten days later I heard back from my surgeon. He went over the films with a respected radiologist and they decided there's nothing to worry about on the MRI. He wants me to rest the hip another 3-4 weeks before attempting some easy exercise.
April 16, 2006
My GP, who was actually the one who ordered the MRI, asked a radiologist expert in bones/joints to also re-read the MRI. This radiologist thinks there may be a problem in the hip joint itself. I am scheduled for another MRI with contrast injected into the hip (arthrogram) along with local anesthetic (marcaine) to help confirm the joint is the source of the pain. I guess the good news is that they may have found the underlying problem that has delayed my recovery for so long. I know it's premature, but I've starting researching minimally invasive arthroscopic hip surgery, which is only performed by a select few orthopedists nation-wide. My experience clearly supports the need to take a very active role in one's treatment. You should handpick your radiologist BEFORE you have an MRI performed. You just CANNOT defer the medical decisions and choices to your doctors. Sometimes you have to question their diagnosis or lack thereof.
April 27, 2006
I did some exercise to aggravate the hip leading up to the exam. When I met with the radiologist before the exam, he actually felt that the arthrogram MRI was unnecessary but he wanted to do the injection into the joint. Bottom line - I felt zero relief after the injection, which essentially all but rules out the hip joint as the source of my current difficulty in tolerating exercise. Back to square one. I made an appointment to see a new orthopaedist in 3 weeks and I'll give him a shot at cracking the mystery.
May 16, 2006
The new (#3) orthopedist said it was either trochanteric bursitis or iliotibial band tendonitis. He said the fracture/surgery may have resulted in permanent issues with the soft tissue to bone interface. First thing to try was a cortisone injection into the bursa, which he duly performed. He recommended stretching of the iliotibial band and trying some walking/swimming in 3-4 days.
May 31, 2006
The cortisone injection into the bursa didn't help at all. #3 orthopaedist seems less definite on what the problem may be and he essentially threw in the towel and told me to just give it time.
I've given up on the orthopedists in the surrounding area. I've contacted highly regarded orthopedists in Colorado and New York City.
I tried exercising easily for a few minutes on a NordicTrack, but the usual hip aggravation set in 1-2 days later.
June 23, 2006
After phone consultations with the Colorado orthopedist, I had another MRI performed at the Hospital for Special Surgery in NYC. They clearly saw significant scar tissue and adhesions between the hip musculature and tendons. I saw an orthopedist there (#4) and he wants to first try physical therapy and if unsuccessful, endoscopic surgery to alleviate the scarring and adhesions. This is probably the problem that started back in October, but failed to be diagnosed by my local orthopedists. He also prescribed an ultrasound-guided injection into the trochanteric bursa. This injection definitely resulted in some relief, and I'm apt to believe that the previous "blind" injection one month earlier missed the mark.
On June 26, I went into physical therapy again and the therapist is using ultrasound and agressive massage (release) therapy in an attempt to break up the scar tissue - also plenty of stretching and hot/cold etc. I'm also seeing a chiropractor who is doing Active Release Technique in an attempt to break up the scar tissue and adhesions. That's 4 therapy sessions per week.
August 1, 2006
The therapy continues. Based on recommendation by a few locals, I saw another orthopedist (#5) who says my case isn't that unusual despite that fact that in my research after my initial accident, I never read anywhere that it can take years to come back from a broken hip and that soft tissue issues were so difficult. He said DON'T go in for more surgery in an effort to resolve the adhesions. He said that I should expect some pain and discomfort and slowly resume physical activity and to try another anti-inflammatory medication.
The next day my active release therapist/chiropractor told me to do yoga and look toward stretching/strengthening my entire body rather than jump into an exercise routine that only worked my upper or lower body. He also encouraged cross-training.
For ten months, I had thought there must be one specific underlying problem that needed correcting and then I would be "okay." I now realize it's going to be a VERY slow road back and I'll have to learn to tolerate some level of pain for some time to come. This was confirmed by the orthopedist on August 1, but none of the doctors up until that time expressed this view. For the first 10 months, none of the doctors brought up the possiblity of soft tissue injury either.
September 7, 2006
I cut back on my therapy to one session of Active Release Technique per week, but have been doing 3 yoga classes per week. The hip finally feels like it is really starting to come back to life. It doesn't feel "normal" like the good hip, but it is feeling strong and capable. I do an occasional vigorous 2-mile hike, although it's ususally a bit sore for a couple of days after. I take 600-800mg ibuprofen when I do experience soreness. I tried a few 5-minute sessions on the bike trainer, but there still seemed to be a residual achiness for a few days afterward. However, on the insistence of my chiropractor, I did an easy 30-minute bike ride yesterday.
September 13, 2006
After a few days, the hip did develop some achiness from the bike ride. I now believe that the hip just won't tolerate repetitve motion with too closed a hip angle (flexing). As an experiment, I started to do some 5 minute sessions of straight-legged jogging since it involves a very open hip angle and little flexing. I also put some very short cranks (152mm instead of 172mm) on my bike and brought the handlebars very high and close so that I'm sitting practically vertical - this is to open up the hip angle and minimize flexing. I did a 30-minute bike ride on the 12th and it was tolerated better than last week, as was the jogging. The yoga classes continue to go very well.
There is a major obvious limitation in my right hip in external rotation. If I sit on a chair with my right ankle crossed on top of my left knee, and let my right knee fall toward the ground - the right knee doesn't fall nearly as far as when this is done with the legs reversed. If I just sit for a minute or two with my right leg crossed like this and relax into the discomfort and try to let that right knee fall further and further, I discover more and more layers of tightness and discomfort. To me, this reveals how much the soft tissues surrounding the hip joint have reprogrammed themselves after the accident in an attempt to protect the joint. Somehow, this must slowly be reversed.
I did a 60-minute easy ride on the 18th and I'm afraid the bursitis/inflammation/stiffness really flared up again two days later. I'm going to put off further attempts at bicycling for a while and work on muscle strengthening in the gym and jogging with fairly straight legs to keep the hip angle open, in addition to the yoga. Perhaps I will be able to slowly increase the jogging to 20-30 minutes and I can get my first meaningful cardiovascular workout in 15 months.
October 4, 2006
The jogging also led to inflammation. I'm going to put off my attempts at cardiovascular activities for the near future and just work on yoga and pilates. I did my first pilates exercise class last night and it should work well with yoga in improving core strength and flexibility. Perhaps the hip needs even more time before cycling or jogging can be pursued.
November 8, 2006
Since things don't seem to be improving with time (the inflammation flared up again last week), I went to see a new physical therapist today who was highly recommended by the yoga teachers in my area. She examined my hip/pelvic alignment and my gait (very messed up) in ways that nobody had previously checked. She believes that the crash caused a significant misalignment of my two hips and resulted in a functional leg length discrepancy, alterations in my gait, and overcompensating (overprotecting) musculature and nerves. There's a tight hip capsule, many weak and tight muscles, and out-of-whack muscular innervation. I've been going for 3 intense, long sessions per week that include some combination of exercises, electrostim (sometimes with solution), ultrasound (sometimes with medication), galvanic ultrasound, electro treatment of trigger points, electro/laser accupuncture, deep tissue work,etc. On days that I don't have treatment, I do about 2 hours of home exercises and stretching that have been assigned. Her approach definitely seems a quantum leap in terms of being more comprehensive, intense, and engaged than any other practitioners to date.
December 12, 2006
For the past year I have been somewhat haunted with the notion of surgically repairing the scar tissue and adhesions. A potential new source of optimism dawned yesterday during my physical therapy session. My therapist was doing some deep tissue massage along the incision scar. Almost out of the blue, she suggested the possibility of having a plastic surgeon open the incision and re-suture each of the tissue layers using absorbable gel sheeting between the layers to prevent adhesions from reforming while healing. This might be the mystery procedure that I've been waiting for, that nobody else previously mentioned. The root of my problem might very well be adhesion between the iliotibial band (ITB) and vastus lateralis (quadriceps) at the site of the incision. I am scheduled to consult with a plastic surgeon in three weeks and continuing with the physical therapy in the meantime.
(postscript: the plastic surgeon told me to stick with an orthopedic surgeon)
December 23, 2006
I am definitely getting strength back into the hip with the 3X/week physical therapy and home exercises. I saw my orthopedist at the Hospital for Special Surgery in New York today. I am going to have him perform corrective surgery in early February - he will open the old incision, remove the scarring, repair a defect (dent) in my quad muscle caused by the old surgery, go up higher into the hip with an arthroscope and clean up the area around the abductor tendon, go into the joint space with the arthroscope and clean up cartilage damage, and finally carefully resuture using a gel compound to prevent additional scarring. In the meantime, I will continue with the therapy/exercises and strengthen my hip further. The hip is tolerating the therapy and exercises well, with just a little baseline soreness - despite the fact that many of the therapy sessions include tissue work that is excruciatingly painful at times. However, long walks (1-2 miles) and swimming still seem to aggravate the hip.
January 15-25, 2007
My continued work with the physical therapist seems to be bearing fruit. The deep tissue work in the gluteal, posterolateral hip, quadriceps and ITB areas is noticeably less painful. I've started using a dense foam cylinder and a 6 inch 1kg rubber ball at home to sit/lie on with my glute/hip region and roll back and forth with body weight - this seems to be really helping and this also is becoming less painful and more pleasurable.
My therapist has identified two additional suspected problem areas, which correlate well with the June MRI report:
1. Scarring of the posterolateral capsule, the ileofemoral ligament to be specific. This would result in a loss of flexibility and difficulty with internal rotation, which is a big problem for me.
2. A bone spur near the origin of the vastus lateralis (quadriceps) muscle, which might be contributing to the difficulty with sustained exercise programs. The spur would be located in the trochanteric region.
I met with the surgeon again and discussed all the problem areas. He should be able to address all of them with the possible exception of the bone spur. He doesn't want to detach any muscles or tendons in order to work on the bone spur at the point and I totally agreed with his assessment.
He has ordered a continuous passive motion machine to mobilize my hip immediately following surgery. I found a Web site which has good information on the types of adhesions that such a device can help prevent. I surely wish my first surgeon had been more aware of these issues. To quote: "this cross-linking can lead to adhesion formation in the soft tissues, stiffness, and the subsequent loss of passive and active motion in the patient." This is exactly what my therapist has been battling to overcome in my hip.
February 11, 2007 - Surgery #3
The surgery was performed Feb.6 in New York and reportedly went well. The minor labral tear was repaired, scarring in the old incision was removed, scarring in the iliotibial band was removed, the noticeable defect in the iliotibial band was repaired, and the inflamed trochanteric bursa was removed. The vastus lateralis (quadriceps) reportedly looked good (palpable defect was actually in the ITB), as did the capsule and other structures. He said the joint itself was in pretty good shape and showed me photos revealing smooth white/pink cartilage. I am wearing a hip brace for a few weeks and using a CPM machine several hours per day as well as a "Game Ready" cryotherapy cold pump for several hours in 30 minute applications. I will probably be on crutches for 2-4 weeks. I feel a bit of soreness from the surgery in several areas of the hip and quadriceps muscle and there is moderate edema in the thigh/knee (I was told this is normal). There is also noticeable "bruising" in several areas, but the surgeon told me that this is just normal staining from post-op blood. I am not on any pain medication. I believe the post-op hip is doing very well.
I wanted to comment on the effect of the anesthetic, especially in light of my experience from the initial surgery back in 7/2005. Knowing that I would be given an epidural, I asked the anesthesiologist to keep any additional sedative to the minimum amount absolutely necessary. I suspect that he ignored my request. Once again, it took about 7 days for me to no longer feel any residual effects of the anesthetic. During a 4 hour period of the night after the surgery, I took 2 percocets. Before taking the percocets, I was out of bed on crutches hopping around the hospital halls. But after the percocets, I went through a 6-hour period of not being able to stand for more than a minute or two without a drastic drop in blood pressure. This was probably due to a combination of the residual effect of the anesthetic, the percocets, and mild hypovolemia (dehydration). The first time I got out of bed early in the morning, I knew I was about to lose consciousness and did so (twice). Gladly, the hospital staff did not make a big deal out of it like my earlier experience 7/2005, and they carried me back to bed and started pumping me full of fluids and tested my blood pressure over the next several hours.
February 20, 2007
The two twenty minute bike trainer sessions are well tolerated, especially in light of my notes above after the 12/30/05 surgery. In the past few days, there's been pronounced stiffness/soreness in the ITB in the lower half of my lateral thigh down to the knee. After several minutes on the bike trainer, the stiffness/soreness is barely noticeable however. I also notice zero subsequent pain, which had been my nemesis for the past 19 months. The ITB soreness has also started to bother me during the night, especially when trying to sleep on my unaffected (left) side.
February 24, 2007
The therapist introduced some resistance exercises (knee/hip extension, ankle pumps) and internal/external rotation (rotational discs). The next day the stiffness/soreness, especially just above the knee and to the outside (lateral) of the knee, was noticeably worse. We backed off on the exercises the next time, but have continued the bike trainer sessions. The surgeon's assistant told me the stiffness/soreness is not unusual and nothing to worry about at this stage. Otherwise, the hip seems to be doing quite well and I've progressed to using only one crutch.
March 2, 2007
The specific stiffness/soreness around the knee started to abate after 4-5 days. The only puffiness left in my leg is above the knee, where there's a little bruising type discoloration undoubtedly caused by surgical blood that has yet to be resorbed. My quads have started to "wake up" and I can take a few tentative steps without leaning too dramatically. Perhaps I'll be able to walk without crutches in about a week. There's still achiness/soreness in several areas of varying qualities, and the therapist has held off on any more exercises other than low resistance cycling.
March 6, 2007
All the puffiness is gone, and my leg muscles are all functioning again. I'm able to walk without limping, and I had progressed to using a single crutch. My therapist thinks my soreness in the ITB and area where my bursa used to be is normal healing. However, yesterday I once again tried some quad strengthening exercises in PT and this aggravated my hip, causing additional soreness in those areas. Other than easy spinning on the bike trainer, I'm going to forego additional exercises for two weeks and for the time being, go back to using 2 crutches. I've been sleeping well for quite some time now - I sleep mostly on my back and sometimes alternate with lying on my left (unaffected) side. I use one weighted pillow by my right foot to help prevent external rotation when I'm lying on my back and one pillow between my knees when I'm lying on my left side.
With this latest aggravation, it's become clear to me that my ITB is going to take longer to recover from the surgery than I imagined. I see the doctor again in ten days and will discuss this.
March 11, 2007
After soft tissue surgery, you're going to feel all kinds of aches and pains of varying quality, intensity and localization. The post op period is a confusing several weeks of not quite knowing if you're getting better or if there's something wrong. The one definite was that the pain I experienced after physical therapy last week was new, more intense, and bad. By taking a break from physical therapy, and religiously using my crutches, some clarity is finally beginning to emerge on all the different aches and pains I've been feeling.
March 16, 2007
I had my follow up post-op visit with my surgeon today. He confirmed what I've been suspecting, that the ITB is going to take longer to recover than I originally thought. He did extensive repair work on my ITB - he had to cut it in order to remove underlying inflamed scar tissue as well as repair the defect in it from previous surgical incisions. He said it is still healing from the surgery, and strengthening work really can't start until after the healing is complete. Inflammation needs to be avoided and he recommended that I take anti-inflammatory medication regularly for now, and to start pool therapy (i.e., physical therapy in a pool). The 20-minute periods of low resistance exercise bike, which were well tolerated during the first 4 weeks, now causes some aggravation so I've stopped. I am still on crutches and will begin pool therapy twice a week.
March 31, 2007
I did three therapy sessions in the pool this week. So far, the hip seems to be tolerating them well. I'm taking Naprosyn regularly and have been icing the hip often during the day and evening and it's sore, but I'm quite hopeful that the pool exercises might get me "over the hump" toward strengthening and losing the crutches. My only regret is that I didn't try pool therapy sooner after this or the previous surgeries.
I'm purposely delaying further attempts at cycling on the trainer and walking without the crutches, to give space for at least two weeks of pool therapy without other activity possibly interfering by causing aggravation. I realize that when I'm walking and using the hip, there are the sensations of strength and of pain, each to some degree. The immediate goal is to get to the point where the hip feels stronger than it feels painful.
I continue to be impressed at what an irritable structure the iliotibial band is and how tricky it is to find and walk that fine line between easy tolerable exercise that can progressively strengthen the hip versus irritating the hip and progressive inflammation.
April 25, 2007
It's been another tough four weeks. After a pool session, I swam 25 yards freestyle with the okay of the therapist. It felt fine at the time, but the hip was aggravated for a week after that. I stopped doing the pool sessions. I started to slowly introduce some walking without crutches. I also decided to start up again with my main physical therapist 3X/week to work on the inflammation as well as strengthening, although I've only had one session at this point. The leg felt good after that session but I made the mistake of doing two minutes of low resistance exercise bike which really aggravated the hip. It seems to be unavoidably aggravated to one extent or another all the time and I'm resigned to that fact. I'd like to get off the crutches entirely in the next week. I did an Iyengar yoga class yesterday and it seemed to go very well, but my body was a bit of a mess this morning and I knew I needed a pelvic adjustment because I had somehow torqued it and I was reminded of the fact everytime I got up from a chair.
May 4, 2007
April 25 ended up being my last day with any use of crutches, so it was 11 weeks total on crutches. On April 30, my therapist introduced some strengthening exercises to my 3X/week sessions. I am seeing good progress on the strengthening and my hip is tolerating it well so far. It's still always a little sore and stiff, but I'm not feeling any new pain after the exercises. I'm also starting to do my strengthening routine at home on a daily basis with therabands. For the first time yesterday, I walked up two flights of stairs. Optimism dawns.
My therapist has forbidden me from engaging in any exercise with repetitive motion until significant strengthening has been demonstrated. In terms of what I've went through over the past 21 months, this makes perfect sense. I'm hoping to be able to try some swimming or biking at the end of the month if all goes well.
May 17, 2007
I had my 3-month postop followup with my surgeon May 11. He tested my hip muscle strength and was both surprised and VERY happy about my progress since the March appointment. He said I should cut back on the Naprosyn, I could slowly begin all activities (bicycling, swimming), and I should expect it to take up to another year(?!) for all hip limitations to resolve.
I've made great gains in the last week in terms of strength and now I'm suddenly going up and down stairs and was able to walk a brisk mile without much subsequent achiness. The hip still has a low level of baseline "soreness" and stiffness. But my activity/exercise has really ramped up in the last couple of weeks. The fact that the achiness never spikes up to a problematic level is a very good sign. I've come to know every subtlety of my hip sensations very well over the past two years.
Another surprising positive sign is that yesterday my therapist intended to do the first session of deep tissue massage on my hip since the surgery. She spent a lot of time on this work about 7 months ago, and it was VERY painful and very obviously needed. However, when she started working on my hip yesterday, it wasn't painful at all and she only worked for a few minutes because it's simply not needed now.
I've also just begun riding the bicycle on the trainer again - I did 20 minutes with a little resistance yesterday. My hip doesn't feel aggravated from it today and I know this would have killed me a few weeks ago.
May 22, 2007
I did a very easy 4-mile bike ride on 5/18 and felt pretty good afterwards. I then did an easy 8-mile bike ride on 5/20. I felt a bit achey the next day and my therapist did some painful massage. It's not feeling so good today and I suspect that once again I have to put off my hope of getting back on the bike soon. I'm going to try some swimming next week down in Florida and we'll see how that goes. It's possible that I may need to start over again and just do some yoga for a few weeks and forego all repetitive motion.
June 3, 2007
I swam 50 yards freestyle last Tuesday and 100 yards on Thursday. Any residual soreness was minimal, and this was very encouraging. Last week my therapist suggested that I ride my bike once per week for whatever distance/effort I wished as long as there was no pain at all. This would allow a week between rides to recuperate with the help of therapy. I rode 16 miles yesterday with moderate effort. I was a bit sore afterward (no surprise) and a bit apprehensive. But it's not feeling that bad today, and this is again very encouraging. I have been diligent with my daily exercise routine, and the hip strengthening seems to be paying off.
June 11, 2007
I got the green light from the therapist to ride again, and did 17 miles 4 days ago. I felt virtually NO soreness afterward and this was a very happy surprise. I did 20 miles two days later and although my butt ached toward the end, there again was no complaints from my hip. I'm 4 months since the last surgery and suddenly (not gradually) everything has turned around in the last week, and is looking very positive toward resuming physical activity at a high level. At the same time, my hip suddenly feels more natural/normal in everyday movements.
June 18, 2007
I'm continuing to do 15-20 mile rides every 2-3 days. Sometimes the hip is a little sore, but no big deal so far. The only thing that's really bothering me for a few days after rides is my neck, which I assume needs to regain some strength. I did one fairly easy club ride and quickly realized that I'm not up for hard efforts yet and best to put those off till next season. An easy half or metric century (solo) by the end of the season is a more realistic goal. The orthopedists have consistently said that it takes twelve months to fully come back from injury/surgery like this, and now I'm finally understanding.
June 29, 2007
The riding continues to go well. I have to be careful of not pushing too hard with too low a pedal cadence or my knees really feel sore afterward. The muscles and lungs are willing/able but the knee tendons need a period of easy miles to get strong. I managed 250 miles of riding in my first month back and I expect this to continue to increase for the next few months. I hope to be doing occasional 50-60 mile rides in August/September.
I did my first yoga class in about 6 weeks and was amazed at how much better the hip felt. Sitting cross-legged on the mat was markedly improved as is standing straight up. I should also mention that I've been able to discontinue physical therapy.
September 29, 2007
I've met my goals back on the bike but I just wanted to mention that my pelvis/SI joint continues to need adjustment every 1-3 weeks by my physical therapist. The symptoms of alignment issues for me are mainly soreness in my hip and perhaps a feeling of a slight discrepancy in leg length from side to side. My therapist is quite expert at getting it back in alignment. There's obviously muscle imbalance or weakness and I need to give this some attention.
October 16, 2007
I've stopped bicycling to give full attention to the muscle imbalance and have started twice weekly Pilates sessions focusing on my legs. During the first session, it was very apparent that I need to retrain my right hip for proper motion - the nerves/muscles had adapted to the injury/recovery in ways that needed to be unlearned.
November 2, 2007
I stopped the Pilates sessions to give full attention to the SI joint instability. I needed to gain awareness of my SI joint's tendency to "go out" on a frequent basis and gain independence from my need to go to my physical therapist to get my SI joint "back in".
I found a great resource on SI Joint problems at www.calindra.com and tried some of the exercises. I had an epiphany soon after - I realized that I was suddenly experiencing absolutely no discomfort when I did some of my routine stretches to the extreme ranges of motion. This convinced me that the fundamental short term problem was the SI Joint. Unfortunately, in my exuberance of feeling so good, I went out for a short gentle jog and messed it up again and couldn't get rid of the discomfort.
A few days later, I spent 3 hours with a yoga therapist who generously shared her experience overcoming SI joint problems. As a result of what she showed me, the exercises she prescribed, and DonTigny's exercises from kalindra.com, I can now do daily stretches and exercises and consistently know when my SI joint is out and get it back in. She also showed me that I can lie down and sense the (in)equality in my leg length myself and objectively see the correction after the exercises (and the felt "pop"). I've held off on any aerobic exercising and the hip is once again feeling very good. So I'm now laying a baseline of health in the SI Joint and hip and will eventually try to slowly add some strengthening and aerobic exercise to the mix. I am getting quite astute at feeling immediately when the SI Joint starts going out, and that's really what I needed.
December 28, 2007
I still haven't been able to resume a consistent program of exercise that involves the affected hip. The hip gets sore and there's significant SI involvement. I'm still searching for a rehab solution.
March 2008
On the advice of my NYC surgeon's assistant, I attempted to begin a regular program of strengthening and stretching of the hip. My hip soon got very sore from the strengthening but I continued with the yoga. I noticed that I started having frequent attacks of lumbosacral (lower back) stiffness and pain and that these attacks were getting worse and worse. I stopped all activity and went to see a different physical therapist to seek relief from my acute back problem. He quickly surmised that the cause of my back problem was unresolved hip issues. He pointed out that my right glutes were significantly atrophied and my ITB was tight. He started with some myofascial release work on my piriformis and glute medius muscles which really seemed to need it. I'm also doing a lot of stretching. Soon I will begin a very gradual program of hip strengthening, focusing on the extensors and abductors.
I also went back down to NYC and saw my surgeon again and his favorite physical therapist for a consultation. It honestly didn't prove that helpful with nothing really new being heard.
April 2008
During a two week vacation break from physical therapy, I was able to walk/hike several miles each day that included a few fairly intense up/down hikes in the desert. The hip did really well. I returned to physical therapy right after I got back. The therapist, for whatever reason, suggested I try several new strengthening exercises during my session. The next day my hip started to ache and over the next two weeks, the hip slowly got progressively worse. In hindsight, I was probably a little overconfident after the hiking during my vacation and my therapist was a bit reckless and we did way too much too fast. I've stopped physical therapy, and I see no point in going back. I stretch my hip religiously every day and I am just waiting for it to return to baseline. It might take a month to do that and this is really slow going. After the hip settles back down, I'll try some easy bicycling. If that doesn't work, I'll stick to hiking.
May 2008
As expected, it took a full four weeks for the hip to settle down. On the advice of a Naturopath, I've started taking a proteolytic enzyme (18 tablets daily of Wobenzym-N). There's a huge amount of anecdotal information on Wobenzym successfully treating injuries, inflammation, scar tissue, etc. The Naturopath also insisted that I ramp up the bicycling much more slowly than I did last June and avoid club rides. I've done very easy 4, 6, and 8-mile rides with two rest days between recently and so far so good.
June/July 2008
I continue to make slow progress. I started June doing easy 10-15 mile rides as well as a fair amount of rigorous hiking. The hip seemed to tolerate the hiking better than the bicycling. I found it hard to determine whether the achiness in my hip 1-2 days after bicycling was getting better or not, so I began to keep a detailed daily log on how the hip felt. I found this VERY helpful because I learned that a lot of the achiness was happening routinely and wasn't cause for concern. By the third week of June I was doing 25-mile rides. However, I still need to take at least 2-3 days off between 25-mile rides to avoid aggravation.
My recuperation is decidedly different that I expected in one specific respect. I expected my hip pain and discomfort to decrease slowly but consistently until my hip felt more or less "normal." I now realize that the recovery is a lot less about feeling and a lot more about function. Even though my hip hasn't been feeling much better lately, I am hopeful that functionally it is getting more and more capable of sustained exercise. Again, keeping the daily log has helped me realize this. Now that I'm doing some regular substantial exercise, the hip "feels" much stiffer. I am diligently stretching it twice daily now and although I've maintained very good range of motion, I can definitely feel the stiffness when I stretch it deeply in certain directions.
September/October 2008
I had an MRI of my hip. It showed that there has been some progressive arthritic degeneration in the hip cartilage evident since the surgery 19 months previously. This was a bit of a shocker since after the surgery I was told that the cartilage looked good. My surgeon things these changes are responsible for my difficulty in resuming a high level of activity. He mentioned that cartilage issues also can manifest as inflammation in the surrounding musculature. He suggested trying other forms of activity to alternate with bicycling, such as swimming. He also said that Active Release Therapy might be helpful (can you say "deja vu all over again"?).
At first, I found this new diagnosis a bit strange because I've had pretty much the same issues for the past 3 years, not just since these changes showed up on the MRI. After mulling it over for two weeks, I am beginning to accept it as a possibility. I can't deny that I was able to put in significantly more miles last year on the bike than this year. But I've made great progress since April/May of this year. So I'll continue and take the cycling as far as it will go. I've started to educate myself about hip resurfacing, but have little interest in going under the knife for a major hip operation again. I did speak with Dr. Su's office - he's one of the leading hip resurfacing surgeons in the USA. They looked at my MRI and said I was definitely a candidate for the procedure and encouraged me to go as far as I can using anti-inflammatories (Naproxen) on a regular basis. They discounted the possibility of liver/kidney issues from the Naproxen as long as my stomach can tolerate it. So I'm taking Naproxen regularly now, and I'm experimenting with shorter/easier rides on a more frequent basis.
For what it's worth, I've cut way back on my stretching and I actually believe this has helped a little bit. Besides a few McKenzie back stretches, I'm just doing hamstring stretches and a little "hips-to-each-side with bent knees" to pop/mobilize my lumbar spine and SI joint. I still feel just as strongly that mobilizing the SI joint is critical.
November 2008
I made a trip out to Syracuse NY and was seen by Dr. Michael Clarke, another one of the leading hip resurfacing surgeons in the USA. He is fairly certain that my exercise intolerance is being caused by some degeneration of my hip cartilage and this was brought on by the hip fracture. He performed a cortisone injection into the hip joint, mainly for diagnostic purposes. It didn't seem to help. The next step with him would be a hip arthroscopy, so that he can see the condition of the joint surface up close to determine whether a resurfacing is indicated.
December 2008
I consulted another orthopedist and read widely about hip resurfacing and it seems that my hip degeneration isn't nearly as bad as would be expected for a resurfacing patient. So I'm not going to proceed down that route at this time. I've joined the local "Y" and will attempt to slowly build up my swimming endurance and see if I can tolerate that as a regular exercise regimen. I am very aware that I have lost so much strength in my leg muscles and this isn't helping my hip at all, so I hope to reverse that.
January 2009
I'm swimming (freestyle crawl) every other day for about 30 minutes. Even though I'm trying to minimize my kicking, the hip still feels a bit sore. So I'm living with a baseline level of soreness and often take Naproxen, but I'm still maintaining the every-other-day swimming routine. I'm already come far in my swimming technique - at first I couldn't swim more than a lap or two without being totally out of breath. But I've had a few lessons and am doing much better now. I haven't gone near a bike since Thanksgiving.
February 2009
I've had a few sessions with a chiropractor who specializes in applied and clinical kinesiology. It seems that there are still ongoing structural alignment issues in the pelvis/SI that are affecting the hip's functionality. There also seem to be some significant adhesions, particularly in the area of the ITB/Tensor Fascia Latae/Vastus Lateralis. This was also called out on my Sept '08 MRI. She did some deep fascial release work on the adhesions and the extreme pain was deja vu all over again.
March 2009
The chiropractic work seems to be helping. I've been swimming a few times a week and I've just started with some occasional short easy bike rides. I realized that I haven't take any ibuprofen in a few months. So there's more optimism on my part that the orthopedists were wrong in simply declaring me a degenerated joint cartilage fait accompli based on my September MRI. This included my surgeon, who in Feb '07 sought to repair my ITB adhesions and now seemed to ignore my September MRI finding that those significant ITB adhesions still existed. I unquestionably still have significant soft tissue issues involving some combination of my ITB, vastus lateralis, tensor fascia latae and piriformis. Fixing those soft tissue issues seems to require mounting a grail-quest type effort considering the state and approach of our modern medical system.
May 2009
I started playing some golf in an attempt to find an activity that would be easy on my hip. After several weeks I began experiencing extreme stiffness in my left mid-back which kept coming back. My new chiropractor told me it's due to weakness and instability in my right hip and right foot. I will be addressing the foot issues with some new orthotics which he feels will really help my hip. He gave me a convincing demonstration of this by doing a tape job on my right foot (heel and ankle mostly) and I was amazed at how my right hip suddenly felt unburdened. He is also having me do some hip exercises, especially to strengthen my gluteus medius. I continue to swim occasionally when my back isn't bothering me. Walking and swimming are about the only activities that my hip can mostly tolerate.
June 2009
I've switched my aerobic workout from swimming to vigorous treadmill walking, varying incline from 8-12% and speed 3.3 - 4mph. I like being able to monitor my heartrate (maintaining ~150bpm), listening to music, and avoiding chlorine. Paying close attention to gait and posture, I think the weight bearing is helping strengthen/balance my hip muscles in ways that swimming or cycling don't touch. I've also started doing regular flexibility/strengthening exercises with an Egoscue workout DVD. The Egoscue method is incredible - it has significant hip and back benefits and helps to restore natural balance and strength in the body.
I've been totally off the bike for over 2 months now and my hip is feeling the best it has since the accident.
August 2009
I traveled to Boston to see a sports medicine physiatrist (MD). After studying my history and examining me, he thought that my problem didn't involve the joint cartilage and suspected a torn tendon that never healed. I am going to follow up later this month with an ultrasound exam to look for the tendon tear as well as platelet rich plasma (PRP) injections to stimulate healing.
update (two weeks later): I purposely aggravated my hip by going for two bike rides. The physiatrist had marked my leg in the spot that overlied the suspected tendon tear. He asked me to aggravate the hip to confirm the spot as the focus of the pain. However I didn't find much correlation between my pain and that spot. Before proceeding with the PRP injection(s), I've decided to first go back to Dr. Clarke with an aggravated hip and repeat the diagnostic injection into the joint to rule in/out the joint as the source of pain (rather than soft tissue). If that test proves negative, I intend to aggressively pursue expert PRP injection therapy.
March 2010
Status hasn't changed - I am doing spinning classes and starting to ride on the road. I anticipate that the hip pain will eventually become constant and I will then return to Dr. Clarke for the diagnostic injection.
April 2010
After about 3 weeks of spinning classes and riding, the hip pain came on in the usual way. It's clear that I can't ride more than maybe once per week. The pain is such that I don't think any doctor is going to localize the source and even if it was my joint, I'm not going to consider more surgery at this point. I'm going to back off from riding as I did last year and focus my attention on trying to develop a barely decent golf game.
May 2010
At this point, I'm pretty much throwing in the towel. There's just too much misery that accompanies an aggravated hip when I keep testing it by bicycling. Golf and hiking will have to fulfill my athletic ambitions. I've decided against pursuing further medical diagnosis or surgery at the hands of always-overly-optimistic physicians.
August - September 2010
Okay, I guess I picked up the towel again. I was seeing a local orthopedist about a different issue and the conversation came around to my hip and I asked him what he thought about me seeing a physiatrist to help with diagnosis. He thought it a good idea and referred me to a physiatrist in their group. I saw him today and I just wish I saw him 3 years earlier (why didn't any of the million orthopedists I've seen ever suggest this?). After reviewing my history, and doing some quick tests he was convinced almost immediately that my problem was NOT my joint ("you'd never be able to effortlessly hop up and down on your affected leg if it was your joint - this is easily ruled out by this simple test") but inflammation caused by the scar tissue between my ITB and vastus lateralis muscle which secondarily is inflaming a bursa in the area. He said the scar tissue is clearly seen on the MRI from '08.
He suggested trying prolotherapy (local injections of platelet rich plasma gel) and arranged for me to be seen the next day by the sports medicine doc in the group that is just starting to do the injections. Wow, what a quick turn-around. I can't help but continue to look back with frustration at the mis-diagnosis by my surgeon in October '08 after the MRI.
So I started riding again, in part to purposely aggravate my hip again to try and localize the areas of pain. For the first 6 weeks, I experienced predominantly stiffness rather than pain. From week 6 onwards, soreness started becoming a bigger component. This progressive pattern is typical of what I experienced in the past. The stiffness and soreness is diffuse and impossible to localize.
So now I'm patiently waiting for the PRP procedure to be performed on my hip. I'm also relieved to learn that the treatment can be applied in a large general area around the hip and it's not necessary that a small anatomical target be identified.
October 2010
The riding was going well although I sensed an underlying progressive stiffness in the hip. Then on one ride, I sensed that something was wrong - getting up out of the saddle and I felt lower back pain/stiffness and I instantly thought of the lower back/SI problems I've had in the past. It seems the exact same progression occurred as back in late '07-'08. I guess it's time to once again to put down the bike and try to address possible underlying muscle imbalance.
February 2011
The PRP injections never happened - the Orthopedic group still needs to lay the groundwork to offer this new procedure. I did spinning classes for several weeks and then the hip aggravation progressed to the point that I had to stop. It's the same cycle repeating itself. I'm not hopeful at this point.
June 2011
I'm on the bike again, but I'm typically giving myself 3 off days between rides, so only riding 1 - 2 times per week and about 30 miles per ride. I'm also using a foam roller for a minute or two on a daily basis to keep the ITB from tightening too much. So the combination of very modest mileage (i.e., lowered expectations) and foam roller is keeping me riding.
September 2011
The Orthopedic Group finally came through and I had the PRP injection Sept 15. The injection targetted an area of soft tissue around the trochanter, using ultrasound for guidance. It was not a painful procedure at all and the hip is just slightly sore the next day. I was told to not exercise the hip for one week and then we'll take it from there.
December 2011
The injection seems to have helped although time will tell. I'm trying to maintain a twice weekly indoor cycling workout regimen.
March/April 2012
Unfortunately, things got progressively worse and I'm once again sidelined with hip and SI joint issues and grasping at straws in order to somehow get my hip issue diagnosed. I saw a new local orthopedist who seemed quite competent but essentially just scratched his head. I'm going to stay off the bike indefinitely. I've started wearing an SI belt full-time and I like the added stability to the hip/pelvis. Hiking the local mountains has become my main physical pursuit.
August 2012
I've been off the bike since March. But I've been able to keep up a consistent routine involving rigorous hiking in the local mountains. Once or twice a week I've been doing summit hikes of 6-10+ miles with up to 2000ft elevation gain. There is some stiffness/soreness but it hasn't progressed or side-lined me.
January 2014
I'm still off the bike and doing rigorous hiking. I've hiked about 130 mountain summits since putting down the bike in March 2012, including hiking throughout last winter. I've experienced no progressive hip soreness from the hiking. In the winter I go to the gym and do either an elliptical or inclined treadmill workout. Even at only two workouts per week, the hip can get sore at times.
Summer 2014
I went a little too hard in June - 8 mile hikes on successive days - and the hip went into an aggravated state for the first time in a long time. I had almost forgotten what this felt like and how annoying it is. Even though the pain might only be a 2 or 3, it is very annoying and not something I want to live with for long. There's definitely a "threshold" effect - once the threshold is exceeded and the hip becomes aggravated, it can take a few weeks or even months for the aggravation to resolve, even with inactivity. This is why I went into a period of just playing golf a few years ago.
I'm happy to say I was back on the trail after a few weeks of resting the hip and once again hiking quite strong in July.
Summary of what I learned:
1. Sports/traumatic hip injuries are often accompanied by soft tissue injuries which are more difficult to diagnose and may prove more difficult to deal with than bone/joint injuries and often take years to heal.
2. The effects of traumatic orthopedic surgery on the soft tissue can be more detrimental to patient progress and recovery than the issue resolved by the procedure itself. It is important to mobilize the hip immediately following surgery to minimize soft tissue problems. This was regretably NOT done for me after my initial hip fracture surgery.
3. Orthopedists are often at a loss at diagnosing and directing the treatment of soft tissue injuries, even those resulting from their own surgical intervention. Many hip orthopedists are not expert at treating sports injuries. Physiatrists (physical medicine MDs) can be your best bet at pinpointing the source of orthopedic problems.
4. Essentially EVERY physician is overly optimistic about outcomes - unfortunately, you must take their predictions with a grain of salt.
5. Physical Therapists vary enormously in their experience and ability to treat complex soft tissue issues. In addition, you need to find a therapist that will devote a lot of time to you - your visits should be measured in hours, and not minutes. You should be given a daily home exercise and stretching routine.
6. If your hip can't tolerate the strengthening exercises in the therapist's office, don't hesitate to find a therapist who's expert in pool therapy and start working with him/her in a pool. You won't believe how beneficial this can be, especially in the beginning while you're still on crutches. It's often hard for the hip to make the transition to suddenly exercising after surgery and resting for several weeks, so go slow and start in the pool.
7. It's crucial to your recovery that you work VERY hard at strengthening the hip. It's difficult to comprehend to what degree the muscles and connective tissues are weakened by surgery and trauma - a MUCH greater degree than inactivity itself. Do not equate the mere absence of pain with recovery. Functionality along with some degree of soreness is VASTLY preferable to a degree of comfort resulting from rest/inactivity. You need to go through several months of some level of soreness while regaining strength and functionality. This was a very important, yet difficult lesson learned through months and months of trial and error without guidance.
8. In parallel with your efforts at strengthening the hip, should be a daily routine of extensive hip stretching. This should continue on a daily basis even after you regain total range of motion in the hip. Along with the hip stretches, be sure to include stretching of the piriformis, ITB, and hamstrings along with stretches that mobilize the SI joint.
9. Patience, patience, patience is absolutely necessary when recovering from soft tissue injuries.
10. After significant trauma and a lengthy period of diminished activity in the hip, special attention needs to be given to relearning proper hip motion in conjunction with strengthening. Strengthening alone will leave your hip's muscles and nerves operating with abnormal compensation that needs to be unlearned. This compensation won't go away on its own, even though your hip seems to have regained its strength.
11. After a hip trauma such as this, there is a high likelihood of SI Joint issues due to the side-to-side imbalance that will ensue in the hip/pelvic/lower back region. Attention much be given to diagnosing the issue, mobilizing the SI Joint through flexibility training, and strengthening the structures to stabilize the SI Joint. There's an excellent discussion of the SI joint mechanics by Neil Chasan, PT
12. In choosing an orthopedist or therapist, you can't be too careful in finding out as much as possible - ask everyone you run into for their input on hip orthopedists or therapists in your area. Get on internet sports and sports injury forums and ask questions and do research. Don't hesitate to see several practitioners until you know you're under excellent care. Really good therapists and orthopedists are really hard to find (really), but they ARE out there, and they ARE really good.
13. MRI machines vary greatly in their image quality and you need a radiologist who specializes in bone/joint issues. Even so, it is extremely hard to get a diagnosis of soft tissue issues on an MRI. You need to exercise just as much care in selecting your imaging center and radiologist. If you possibly can, go to the Hospital for Special Surgery in New York and have Hollis Potter conduct/read the exam.
14. Don't hesitate to go outside your local area for health care if you must, in order to find excellent practitioners. Along the way, I consulted with orthopedists in Colorado, Tennessee and New York City as well as my local area. I travelled 150 miles roundtrip twice a week for Active Release Technique sessions.
15. You need to be quite disciplined about eating habits due to almost total loss of all physical activity. I was able to maintain my pre-fracture weight throughout, but it meant eating A LOT less.
16. Some people (me) are sensitive to the effects of anesthesia. It seems difficult to convince anesthesiologists to lower the dose. For sensitive individuals, it's probably best to avoid all opiate pain medication, especially for 72-hours post-op. I can routinely feel the effects of general anesthesia for a full week after surgery.
17. Proper foot support (orthotics, etc) is important in order to regain proper side-to-side balance after hip injury. Your body will go through various stages of compensation while recovering and having any foot or knee issues may stall the recovery in a compensated/unbalanced state.
18. Ride with adequate hip padding/protection to avoid ever having to go through this. I've experimented with various padding solutions since my accident and the following is what I currently use - this combo is actually not bulky, quite comfortable on both recumbent and racing bikes, provides excellent impact/abrasion protection, and moves well with your legs:
Links to other hip fracture recovery journals:
Links to other hip injury information: